Which anticoagulant is best?

We've spoken about the role of blood thinners to reduce the risk of stroke in patients with AF. If you had AF in the year 2010, the decision was pretty straightforward- warfarin was by far the most commonly used blood thinner in the vast majority of AF patients who required this. It is very effective at reducing stroke risk and is still the drug of choice in patients who have specific heart valve disease. But it comes with inconveniences- patients are required to have regular blood tests to check their 'blood thinness level' (or INR) to ensure their levels stayed within the right thresholds and their dose would have to be titrated up or down regularly to achieve this.

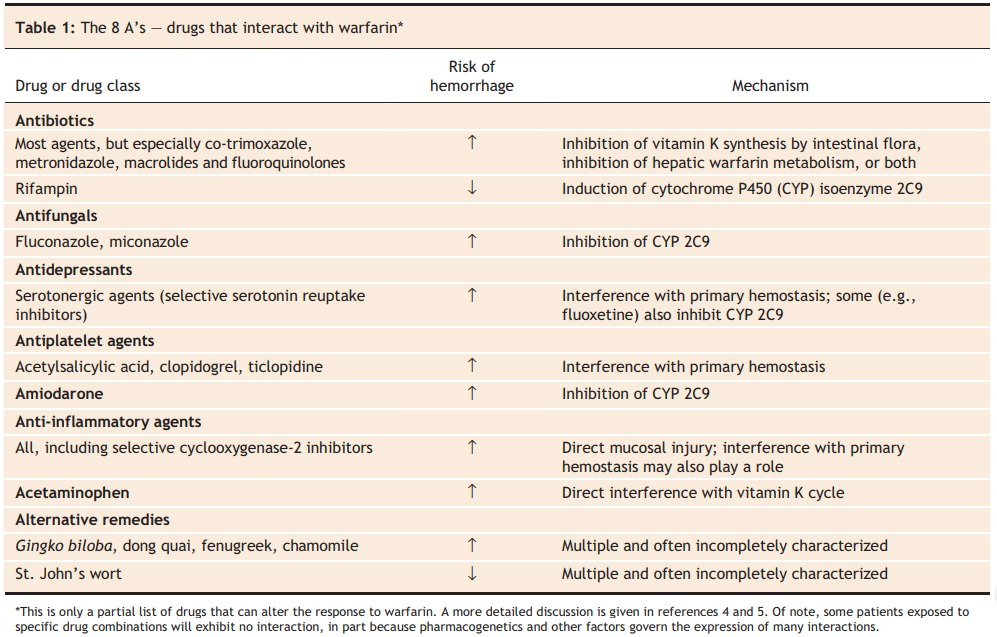
Warfarin also interacts with a number of drugs, including antibiotics and anti-platelets, so it requires close monitoring to ensure the levels are just right.
In the 2010s, new drugs came on the market that seemed to be able to achieve the same degree of blood thinness but were remarkably free of the drug interactions and need for monitoring that many patients taking warfarin found difficult. By name, the 4 most commonly prescribed are apixaban, rivaroxaban, edoxaban and dabigatran.

These were initially called 'NOACs'- 'novel oral anti-coagulants' as a group and now, 10 years on are no longer novel and so called 'DOACs'- direct oral anti-coagulants. As well as their convenience, we have 12 randomised controlled trials of more than 100,000 patients randomised to receive a DOAC vs warfarin. Patients taking a DOAC showed a lower risk of life-threatening bleeding and so this evidence of greater safety now makes them the first choice blood thinners in patients with non-valvular AF.
What about amongst these four? Which is the best? As an evidence-based blog, the truth is we don't have any clear evidence from head-to-head comparisons that one is better than the other at reducing stroke risk in AF patients. Doctors have their own preferences based on familiarity and experiences with Rivaroxaban most commonly prescribed in UK/USA. Many regions have negotiated discounted rates from the producers and so use a specific one for cost reasons.
There are some groups of patients who may benefit from one agent more than the other:
2 vs 1: Apixaban and Dabigatran come in twice a day formulations whereas rivaroxaban and edoxaban are once a day. Again, there isn't clear evidence to support this practice but if a patient might struggle to remember to take their second daily dose, perhaps a once a day regimen is better.
Kidney disease: Rivaroxaban, edoxaban and apixaban may be cautiously trialled in patients with chronic kidney disease (GFR level of 15-30ml/min). All DOACs are contra-indicated in patients with severe kidney disease (GFR less than 15).
High bleeding risk: Dabigatran is available in a reduced dose formulation and can be considered in patients who are at high stroke risk but have a high bleeding risk or a history of bleeding also. Although the DOACs haven't been compared head-to-head, from their comparisons with warfarin, apixaban had the lowest risk of gastro-intestinal bleeding. In patients taking anti-platelet medicines like aspirin after a coronary stent for a heart attack, rivaroxaban has been shown to work well alongside these medications.
Although we've discussed many nuances, the right anticoagulant is the one you take...i.e. don't forget to take your doses if you have been prescribed it. This is especially important in the weeks before and after catheter ablation. The choice of drug is secondary and should be based on the recommendations of your prescribing doctor.
Insider tip: if you have a lot of questions about your DOAC, the risk:benefit ratio and the decision-making process there are specialist pharmacists or anticoagulation clinics run by pharmacists who are incredibly knowledgeable. They often know the intricacies of these medications and the trials in detail and so can be a valuable source of knowledge!
