What can an echo add in Atrial fibrillation?
Learn how an echo, an ultrasound-based imaging assessment of the heart, can provide valuable information for the management of atrial fibrillation. Find out what your doctor is looking for in your echo results and how they can influence your treatment plan.
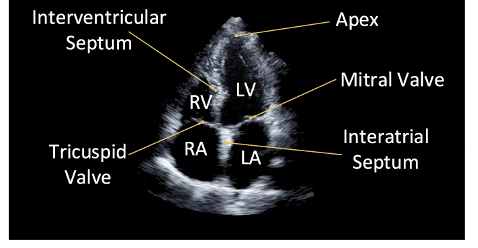
An echo is an ultrasound-based imaging assessment of the heart. It looks at the structure and function of the different chambers of the heart and is a core feature in the assessment of every patient with atrial fibrillation (AF).
But why? AF is a rhythm disorder seen on ECG, so why do you need to have a structural/function assessment of your heart as well? Especially if it means extra trips to the hospital and extra costs to the NHS?
It can broadly be divided into two main reasons:
1.To look for features that would alter the approach to AF management (for example, things that might suggest you shouldn't use specific AF drugs)
2. To look for stratifying features (these are things that might suggest an increased risk of complications, guide how urgently the AF may need to be treated or the likelihood that a treatment may work)
There are 3 key things your doctor will be looking for in the echo (so remember to ask about these, and how they might influence your treatment plan!)
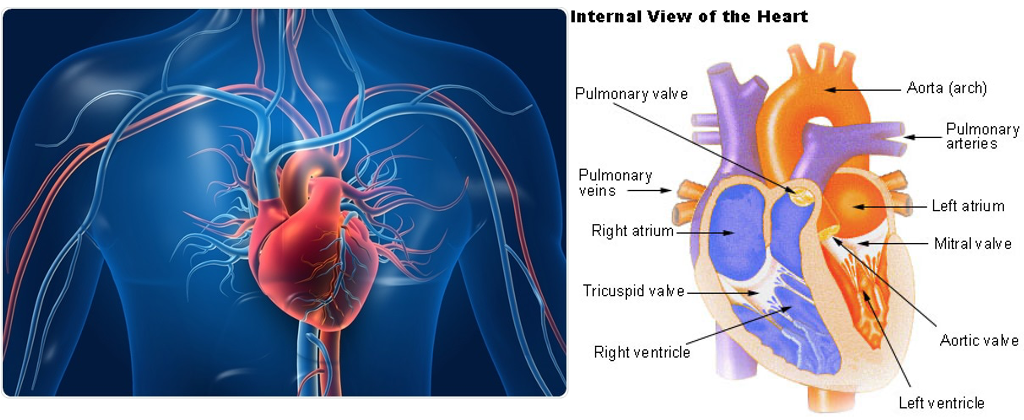
i. Left ventricular (LV) chamber size and function: This is the main chamber of the heart. AF and LV chamber dysfunction have a 'chicken and egg' relationship. LV dysfunction can increase the risk of AF and vice versa. Similarly, there are heart diseases that cause a dilation of the LV which also increases the AF risk and vice versa. This is one of the most significant findings you can make in AF patients because it may increase the urgency of AF treatments and may require urgent drug treatments too. There are also some AF suppression drugs that are usually avoided in patients with LV dysfunction so it's important to know this before commencing drugs like flecainide. So this is a little bit of reason 1 and a little bit of reason 2.
ii. Left atrial size: This is largely for reason 2. The size of the top left chamber correlates closely with how long the AF has been going on for. Additionally the more it dilates, the less likely it is that the AF can be reversed. The normal volume values are 15 − 42 mL/m2 for men and 15 − 39 mL/m2 for women (these are 'indexed values' which means they are adjusted for the size of the person.
iii. Valvular disease- we have covered the INVICTUS trial before- which suggested warfarin should be the anticoagulant of choice in patients with valvular AF. There are 4 valves in the heart (these are one-way gates that maintain a one-way system of blood flow) and when they become stiffened or leaky they can cause changes in the pressures and shape of the heart chambers that can increase AF risk and make it harder to reverse. So identifying valve disease can affect the choice of anticoagulant and suggest the reversibility of the AF in some cases too.
There is also a different type of echo called 'transoesophageal echo'. This ultrasound probe can be passed down the food pipe to view the heart from behind. This is a better way to look for blood clots in the heart and may need to be done before a cardioversion or ablation procedure in high-risk patients; with procedures potentially canceled if this can't be done.
Cardiac MRI is an imaging test that also provides a high-definition structural and functional assessment of the heart. It can help with both reasons 1 and 2- but at the moment, the clinical advantage over an echo is unclear. It's something we're looking at in the AFHF study though, so watch this space!
