Atrioesophageal Fistula after AF Ablation

An In-depth Look at an Extremely Rare Complication
Introduction:
Risk and the POTTER-AF study
Healthcare involves navigating risk: benefit decisions to deliver the outcome the patient wants. This occurs from the start- deciding to go to the hospital (the risks of waiting to be seen, the discomfort of blood tests and examinations, the risk of infection from a neighbouring patient) to the more obvious risk:benefit trade off's like having surgery or an ablation procedure.
The doctor's role is to help a patient navigate this process and preecribe or deliver the treatment chosen. To make good decisions, it’s important to be transparent about the benefit (chances of success, possible outcomes) and risks (possiblr complications, side effects, chances of it not working) of different choices. In healthcare, a patient is allowed to make the decision they want, even if others don’t agree with it as long as it’s an informed decision- ie the patient is aware of the options and the risks of treatment as well as non-treatment.
Here is the consent form used at our hospital, St Bartholomew’s Hospital, the largest ablation centre in Europe. The benefits and risks are detailed and the probabilities are based on International and local reviews of our cases (we audit our AF outcomes and complications every couple of months and discuss them as a group in a non-judgemental manner.)
The form and the related discussion can be pretty overwhelming, especially if not conducted sensitively with clear explanation. In the Risk section, it states damage to the food gullet as a reference to - atrioesophageal fistula (OF). It’s the most serious possible complication of AF ablation but also incredibly rare. Most cardiologists will go their entire careers without seeing one. It’s so rare in fact that it’s very hard to collect good data on it. And without good data, we can’t understand the risk of it ourselves as doctors but importantly we can only offer patients vague estimates of something so rare.
As a result of international collaboration and accurate record keeping we potentially have a way to overcome this. If you gather all the records from many of the high-volume cardiac centres from around the world you can generate big data- hundreds of thousands of ablation cases over many years. And looking at the data at this scale, you can start to see possible patterns that wouldn’t be possible to measure in any single country's data accurately.
The POTTER-AF study did just this for OF. Based out of Lubeck, Germany, Prof Roland Tilz and colleagues took on this challenge. I was appointed to submit the Bart’s data (thousands of cases over many years!), so I had a first-hand view of just how much effort this was. It was a huge undertaking coordinating and managing data from 214 centres from 35 countries. It was presented at EHRA 2023 (the pan-Europe arrhythmia conference) and published in the European Heart Journal earlier this month so we can now talk officially about the results.
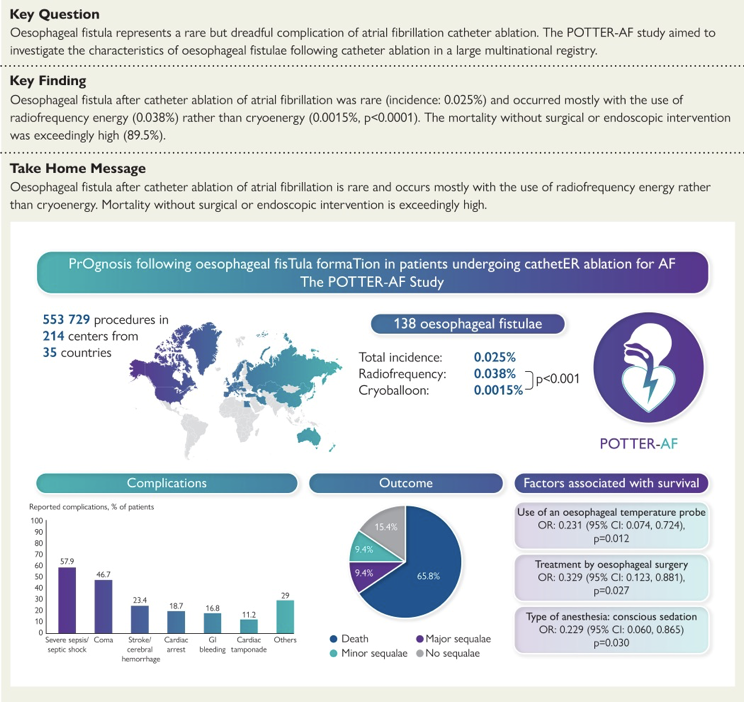
The data from more than half a million ablation cases confirmed what we thought- OF is incredibly rare. a 0.025% chance or 1 in 4000 risk. Before talking about OF and the learnings further, I want to take a tangent to talk about risk and put that number into context.
Framing the Risk
Risk, by its very nature, is a concept filled with uncertainty. It quantifies the possibility that something may happen. But when we talk about risks in the realm of healthcare, particularly with regard to rare complications of medical procedures in a list, understanding it in perspective can be difficult.
If we take the risk of developing an oesophageal fistula after AF ablation reported in the POTTER-AF manuscript, this complication occurs in approximately 0.025% of cases. What does a 0.025% chance look like in the real world?
To put it in perspective- consider how you view the odds of being struck by lightning. Over the course of your lifetime, the chances of this happening are roughly around 0.033% - a higher risk than developing an oesophageal fistula after AF ablation.
Another example of a similar ‘risk’ is that of finding a four-leaf clover. The chances of stumbling upon one is approximately 0.01%- lower than the chance of developing an oesophageal fistula.
The aim of these examples isn't to downplay the seriousness of an oesophageal fistula; rather, it is to try and get an appreciation of the rarity of it before we go on to talk about it further. It is a risk, yes, but very very low likelihood.
What is an Atrioesophageal Fistula?
AF ablation involves delivering energy to the left atrium- the top chamber at the back of the heart. This is done to break the AF circuit and block the areas it comes in from.
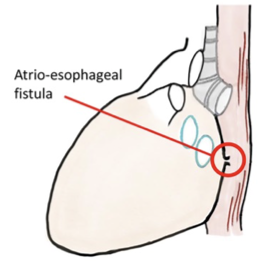
The left atrium sits adjacent to the oesophagus- the food pipe. The walls touching. If the procedure's energy inadvertently affects the oesophagus, it can potentially lead to the formation of an oesophageal fistula, which is an abnormal connection between the oesophagus and another structure, in this case, the heart. This isn’t an immediate event- it’s not poking through the back wall of the heart, it occurs by sustained irritation of the back wall of the atrium and the front wall of the oesophagus so a connection erodes over time- days to weeks. The risk is then of blood leaking into the foodpipe or air from the foodpipe entering the heart and blood circulation causing complications.
Risk Factors for Oesophageal Fistula
Even with the >500,000-case dataset of POTTER-AF, the raw number of events was still quite low. But there was some signal to help identify features that may marginally increase the relative risk.
Firstly, the type of ablation energy used may play a role. The study found that the use of radiofrequency energy, as opposed to cryoablation, was associated with a slightly higher incidence of oesophageal fistula. This was possibly due to the more intense heat generated by radio-frequency energy. But remember, we’re only measuring one complication here and the risk of other complications and the potential benefits of one energy type versus another were not considered in this study.
Secondly, anatomical considerations can also matter. Patients with naturally closer proximity between the left atrium and the oesophagus may be at a marginally increased risk. This is a tough one because it isn’t a factor controlled or predicted by the patient or the physician. There has been some investigation of oesophageal probes you can put down the foodpipe when the patient is asleep, but these haven’t shown any benefit.
Lastly, the skill and experience of the physician performing the procedure can also impact the risk. As with any procedure, the risk of complications tends to decrease as the physician's experience with the procedure increases.
Again (like a broken record), I must stress that the risk even in the context of all these risk factors is still incredibly low. And looking at data in this retrospective (looking backward at data reports) way makes it difficult to draw conclusions or suggest causation. The POTTER-AF data has suggested associations and it shouldn’t be used to say something is the cause.
Recognising Red Flag Symptoms 🚩
Of the patients who developed an OF, there were several key symptoms. Again, they aren’t specific to OF, and in the vast majority of cases, patients experiencing these symptoms after an AF ablation will not have an OF. But they are considered “red flag” symptoms and should prompt an evaluation by a medical team to be able to rule it out.
- Fever: This was the most common symptom- seen in almost 60% of cases, potentially due to inflammation and infection due to bacteria moving into the heart. An unexplained or persistent fever following an AF ablation should prompt medical evaluation. Remember symptoms would usually occur weeks after the ablation procedure so patients should remain vigilant through the first month.
- Neurological symptoms: This may include sudden weakness, numbness, or difficulty speaking. These symptoms might suggest a stroke, possibly due to air or other particles from the oesophagus to enter the bloodstream and reach the brain.
- Chest pain or discomfort: While some chest discomfort is normal following an AF ablation, severe, worsening, or persistent pain should be reviewed.
- Difficulty swallowing or pain during swallowing: These symptoms could suggest damage to the oesophagus but is also may be a result of intubation procedures or a transoesophageal echo if the ablation was done under general anaesthetic.
- Blood in vomit or stools: This can be a sign of internal bleeding and should seek medical attention to determine the cause.
Management Strategies for Oesophageal Fistula
The numbers reported even in a study as large as this are low. And the severity of OF can vary, so it’s hard to make any comparison between different strategies. What was clear though was that getting medical attention early was associated with better outcomes. Early presentation to a medical team who is aware of the possibility of OF, leads to earlier investigation, detection, and potential treatment.
Diagnosis is with a CT scan. Contrast is given to try and make the diagnosis and pinpoint the fistula site. Whereas some cases had an endoscopy (camera down the food pipe) to try to visualise the OF, avoiding passing instruments down a foodpipe blindly may risk poking and making things worse. But again, the data isn’t strong enough to say anything conclusively.
Once diagnosed, antibiotics were usually given with is a rationale initial step if there was a concern of bacteria passing into the bloodstream.
The treatment decision is then largely between endoscopic repair (passing tools down the foodpipe) or surgery. We can’t say one is better than the other, it’s likely sicker patients received surgery and so you can’t compare the two. But the treatment decision should not be made hastily. Multiple experts- cardiac surgeons, imaging doctors, electrophysiologists, endoscopic doctors should consider the options and present personalised treatment options or plan to the patient after much consideration.
Conclusion:
Safety and Efficacy of AF Ablation
We’ve spoken a lot about risk and complications but I want to end by discussing the other side of the coin- the benefit. No procedure is without risk and these risks are balanced by the outweighed potential for benefit. AF ablation is the most effective way of reducing the severity of AF symptoms. Many patients with untreated AF can suffer a poor quality of life, symptoms of dizziness, fatigue, or debilitating palpitations. But not all patients. This is why it’s important to be clear about why you’re having ablation and have discussed that with your doctor.
That’s why your cardiologist may suggest against ablation if you have no AF symptoms nor heart weakness. Even a very very low risk of complication is hard to justify if there is absolutely no benefit on offer.
While the chance of this complication is extremely low, it's crucial that both physicians and patients are well-informed about it, prepared to recognise it, and understand how to manage it if it does occur. Understanding and communicating about such low-probability, high-impact events can be challenging. They can induce anxiety or deter patients. There is continued efforts to drive this risk even lower using technology. Catheter evolution and mapping systems are being continuously iterated to calibrate the energy delivery and give the operator feedback about the extent of each treatment being applied. Having a reliable reference when discussing this oesophageal fistula with patients is a significant step forwards for clinical care and research to try and improve the safety profile of catheter ablation further.
Tilz RR, Schmidt V, Pürerfellner H, Maury P, Chun KJ, Martinek M, Sohns C, Schmidt B, Mandel F, Gandjbakhch E, Laredo M, Gunawardene MA, Willems S, Beiert T, Borlich M, Iden L, Füting A, Spittler R, Gaspar T, Richter S, Schade A, Kuniss M, Neumann T, Francke A, Wunderlich C, Shin DI, Grosse Meininghaus D, Foresti M, Bonsels M, Reek D, Wiegand U, Bauer A, Metzner A, Eckardt L, Popescu SȘ, Krahnefeld O, Sticherling C, Kühne M, Nguyen DQ, Roten L, Saguner AM, Linz D, van der Voort P, Mulder BA, Vijgen J, Almorad A, Guenancia C, Fauchier L, Boveda S, De Greef Y, Da Costa A, Jais P, Derval N, Milhem A, Jesel L, Garcia R, Poty H, Khoueiry Z, Seitz J, Laborderie J, Mechulan A, Brigadeau F, Zhao A, Saludas Y, Piot O, Ahluwalia N, Martin C, Chen J, Antolic B, Leventopoulos G, Özcan EE, Yorgun H, Cay S, Yalin K, Botros MS, Mahmoud AT, Jędrzejczyk-Patej E, Inaba O, Okumura K, Ejima K, Khakpour H, Boyle N, Catanzaro JN, Reddy V, Mohanty S, Natale A, Blessberger H, Yang B, Stevens I, Sommer P, Veltmann C, Steven D, Vogler J, Kuck KH, Merino JL, Keelani A, Heeger CH. A worldwide survey on incidence, management and prognosis of oesophageal fistula formation following atrial fibrillation catheter ablation: The POTTER-AF study. Eur Heart J. 2023 Apr 16:ehad250. doi: 10.1093/eurheartj/ehad250. Epub ahead of print. PMID: 37062040.
