Surgical AF ablation
Atrial fibrillation can be treated by targeting the area it originates from- the top left chamber of the heart and the pulmonary veins. The most direct way of treating this region is through cardiac surgery. And that's how AF used to be managed before the advent of catheter ablation and for some patients today, that's still the right option...

Before Catheters, There Was the Knife.
Catheter ablation is the most effective method for treating symptomatic atrial fibrillation. However, before the art of electro-anatomical mapping and radio-frequency ablation techniques, AF was treated surgically.
The Cox-Maze procedure was developed by Dr. James Cox in 1987. A series of strategically placed incisions in the heart's top chambers were made to create a "maze" of scar tissue- also referred to as the 'cut and sew' method. These scars acted as barriers to the electrical impulses through the heart and tried to prevent the chaotic AF-related signals from taking over.
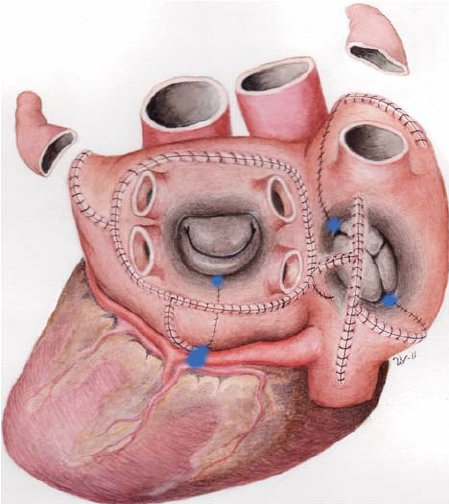
Over the years, the operation underwent several refinements, culminating in the Cox-Maze 4 method. This procedure is a more advanced version of the original Maze, incorporating cryoablation (freezing) and radiofrequency ablation to create the necessary scar tissue, rather than repeated incisions.
The Role of Surgical Ablation Today
Surgically delivered ablation lines are robust. The lines of block are solid and irreversible. However surgical ablation is not a light undertaking. Although Cox-Maze 4 can be done through keyhole surgery, it still is major heart surgery that requires a surgical team and carries the risks of heart surgery too.
With the advent of catheter ablation, one might wonder if there's still a place for surgical ablation in today's world. The answer is yes, but its application has become more specific. Surgical ablation is now considered in two particular circumstances:
- Concurrent Cardiac Surgery: If a patient is already undergoing heart surgery for another reason, such as valve replacement or bypass, it may be advantageous to perform surgical AF ablation concurrently. If you're having to access the heart for one reason, it makes sense to take advantage of that access and consider performing an ablation via that route as you're undertaking the risks already.
- Persistent and Long-Standing Persistent AF: We know that catheter ablation has a high success rate in patients with paroxysmal AF and is also quite good in early persistent AF. However, we also know the longer the AF is entrenched, the success rate reduces. Especially if catheter ablation has already been attempted, the law of diminishing returns kicks in. If AF remains a significant burden and medical control is proving difficult, surgical ablation can be considered in patients who are good surgical candidates and this is recommendation is endorsed by International Guidelines globally.
The Convergent Procedure - A Promising Hybrid Approach
The convergent procedure is an innovative hybrid approach that aims to combine the best of both worlds - surgical and catheter ablation. This technique involves a minimally invasive surgical procedure to create scar tissue on the outside of the heart, followed by catheter ablation to address the inside. The layout of the heart in the chest means the surgical approach is very good at treating the body of the left atrium and can deliver very good treatment to the back wall. However, catheter ablation from the inside may be a better approach to target the pulmonary veins and thus the convergent procedure combines the strengths of both approaches.
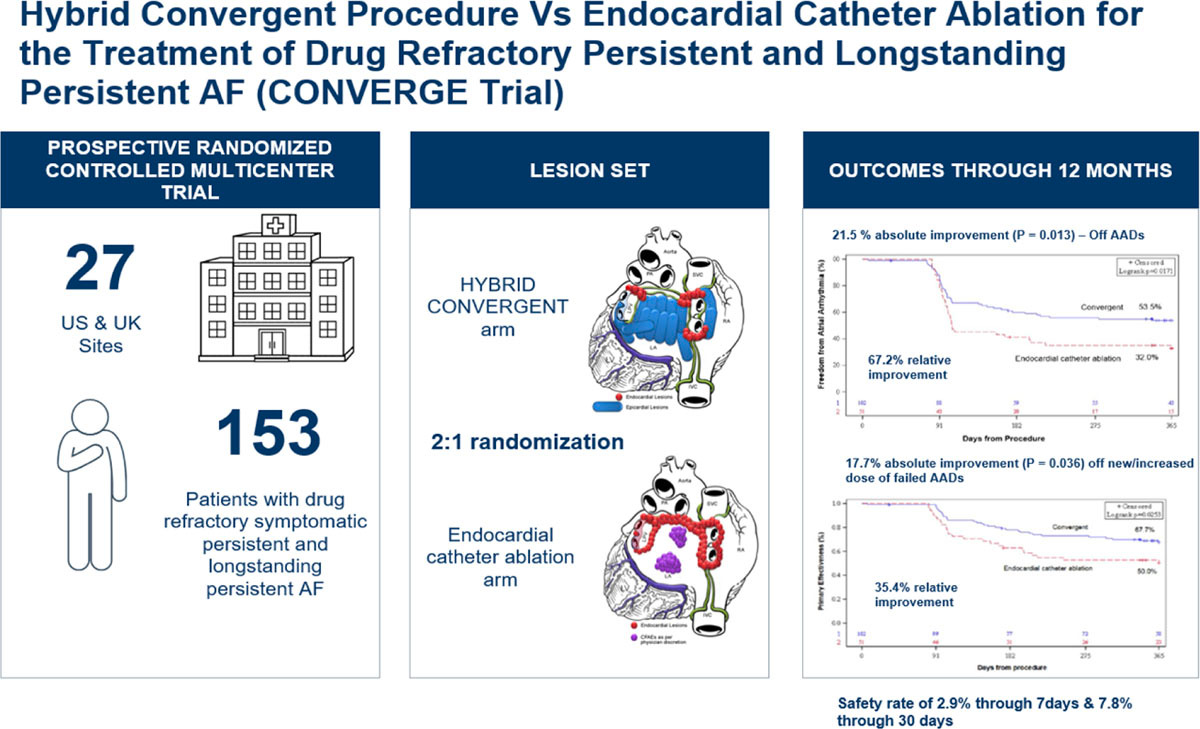
The CONVERGE clinical trial compared the hybrid procedure to catheter ablation alone and although it was a small study of 153 patients, it was performed in a randomised controlled method (a strong statistical trial design). The study enrolled patients with persistent and long-standing persistent AF i.e. patients with more entrenched AF.
The results showed a greater proportion of patients were free from AF at 12 months after hybrid ablation versus catheter ablation alone (67.7% versus 50.0%) but conversely, this means about a third of patients still had a recurrence despite the two procedures. Whether this superiority justifies the risks and prolonged recovery after surgical ablation is a personal decision and is something that each patient who meets the criteria must consider with their healthcare team on an individual basis.
Conclusion: A Nod to the Past, with an Eye on the Future
Surgical ablation will continue to improve. As surgical techniques and tools get better (and our understanding of AF mechanisms), there is no doubt that this efficacy rate will increase and the approach will become more attractive. For patients undergoing cardiac surgery anyway, having a surgical ablation is very reasonable. Having a diversity of treatment options is important to be able to offer patients alternatives and if we can personalise AF types more precisely, we may be able to identify the groups of patients most likely to benefit from treatments to the areas that surgery can reach.
DeLurgio DB, Crossen KJ, Gill J, Blauth C, Oza SR, Magnano AR, Mostovych MA, Halkos ME, Tschopp DR, Kerendi F, Taigen TL, Shults CC, Shah MH, Rajendra AB, Osorio J, Silver JS, Hook BG, Gilligan DM, Calkins H. Hybrid Convergent Procedure for the Treatment of Persistent and Long-Standing Persistent Atrial Fibrillation: Results of CONVERGE Clinical Trial. Circ Arrhythm Electrophysiol. 2020 Dec;13(12):e009288. doi: 10.1161/CIRCEP.120.009288. Epub 2020 Nov 13. PMID: 33185144.
