Should I stop my blood thinner after ablation?
"Even though your AF ablation was successful and we have not seen any AF in the last 12 months you should continue your blood thinner for the rest of your life…"
When I started my Electrophysiology training I remember thinking this had to be a defensive medicine/medico-legal position rather than evidence-based. I thought the reason electrophysiologists made this recommendation was because we had not done the Studies to show the risk of stroke goes back down. I thought we lacked the proof to say it was okay rather than there being any actual risk after a successful AF ablation.
If atrial fibrillation causes strokes
And we have treated the atrial fibrillation.
Then surely we have removed the risk of stroke?
However, when I dove into the data I realised that both of the fundamental tenets of this argument were potentially wrong. So in 2019, we published our critical review of this question in the European Journal of Arrhythmia and Electrophysiology.
Five years on this is still one of the most common questions asked at follow-up after ablation. In the final sentence of that article, I wrote-
we [doctors] will have to continue to be honest and tell them [patients] that at the moment no one knows what is correct and to do our best to help them make a decision that they are comfortable with.
The error was only publishing this in a medical journal to be read by Cardiologists. the patient is the decision-maker, they should understand the rationale as well. So let’s review the problems with the two fundamental tenets of the logical argument.
Tenet 1: We have treated the atrial fibrillation
After an ablation is the AF really gone?
The likelihood of AF recurrence reduces as time goes on after successful catheter ablation. Freedom from AF at the 12-month time point represents a significant milestone. The risk of symptomatic AF recurrence after this time point is small. (I’m intentionally avoiding numbers/percentages because this depends on individual risk factors)
However, we know that asymptomatic AF episodes can also occur from our studies of patients with monitoring devices like pacemakers and implantable loop recorders. These episodes still increase the risk of stroke even in the absence of symptoms.
As a side note- I am presenting some new data on risks in asymptomatic patients next week at the Heart Rhythm Society meeting in Boston- so more to come on this soon!
So the challenge is making lifelong treatment decisions based on a couple of spot checks for Afib in the first 12 months. We have quite a lot of data from International registries that show the rate of stroke in patients after catheter ablation is low.
Studies compare the stroke risk to patients who don’t have catheter ablation or to patients who do have catheter ablation but stay on their blood thinners due to recurrence or other risks. So it can be hard to interpret the results for our purposes. The follow-up period is usually short (only a year or two) and still doesn’t tell us if the risk is low enough to stop the blood thinner entirely.
We have some data from a few European and American centres that have discontinued blood thinners in patients after their AF ablation and reported a low rate of stroke. The largest study of this type involved 3355 patients who were switched from a blood thinner to aspirin at 4 months. These patients had a low risk of stroke- there were 2 events over 2 years, representing a 0.07% risk. But again the study had its limitations- any patient with AF recurrence was excluded. Any patient with abnormal atrial function (upper heart chamber) on echo was excluded. Patients were only followed up for 2 years and so it is hard to make decisions about lifelong therapy from this alone.
However, they are structured in the same way- patients are considered AF-free if they have no episodes in the first 6-12 months and then the rate of stroke over 1-2 years of follow-up is reported in the study. The one study that followed patients out to 10 years showed that by this late time point, there was no difference in the rate of stroke between patients who remained in AF or normal rhythm at the 12-month time point.
The React-AF trial
But what if we could better identify when AF recurrences happen (or don’t happen) over the long term)?
We can use heart rhythm monitors like the Apple Watch to detect AF episodes. And so, if AF causes the stroke risk, we can limit the timing of blood thinner usage to the window of effect around each episode. And so REACT-AF was launched in 2023. Hoping to enrol 5350 patients with paroxysmal (intermittent) AF and an Apple Watch to detect their own episodes from home. Patients are randomised to either use their blood thinner continuously (the norm) or to a ‘pill-in-the-pocket’ regimen where they only take blood thinners if an AF episode happens and for 30 days after and then stop (if they are subsequently AF-free). This study isn’t limited to post-ablation patients either so the results will be more widely applicable too..
However, the inclusion criteria are quite strict- in that patients are expected to wear their smartwatch for at least 14 hours/day and have a CHADSVASC score between 1 and 4.
REACT-AF has enrolled 300 patients as of February 2024 and expects to complete in 2029.
Tenet 2: Atrial Fibrillation causes strokes.
Patients with AF are at higher risk of stroke than those without AF. And the more AF you have, the greater your AF stroke risk. But does a catheter ablation sufficiently reverse the stroke risk enough to stop the blood thinner?
If you do an ultrasound scan of the heart (an echocardiogram) during Atrial Fibrillation you will see that the upper chambers of the heart do not contract. When the upper chambers are static, blood can clot and float up to the brain causing a stroke.
After a successful AF ablation, the heart rhythm returns to normal, but in some people, the size, shape and function of these upper chambers may not. The electrical problem (that causes the symptoms) and the structural problem (that causes the stroke risk) may not respond in the same way.
The atrial myopathy hypothesis
This has led to an alternative hypothesis emerging in recent years- whether in some patients, AF could just be the electrical marker of an underlying structural heart disease (an atrial myopathy). In this case, an AF ablation might reverse the electrical marker but does not reverse or halt the structural myopathy, meaning the stroke risk would remain.
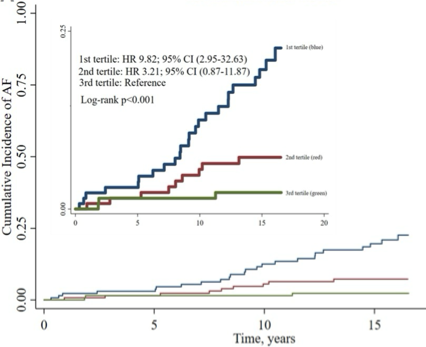
Individuals with an atrial myopathy are at a higher risk of stroke, even without an AF diagnosis.
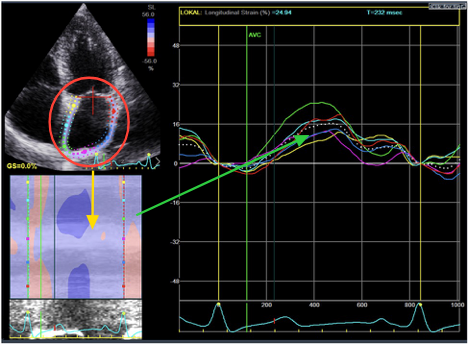
We are seeing this in the AFHF study too. In some patients, the heart may strengthen when the rhythm is corrected but the size and function of this upper left chamber may not normalise.
Patients with an atrial myopathy are a higher risk of developing AF too. This supports the hypothesis that when we see atrial myopathy in patients with AF, the structural disease may have been the preceding insult. It may be cause rather than effect.
And so the only way to be able to settile this is with a randomised controlled trial. This trial design takes the selection bias out of the question and will directly address the question- do patients who stop their blood thinner after a successful AF ablation have a higher risk of stroke than those who continue it…
The Ocean-AF trial
The “Optimal Anti-Coagulation for Enhanced Risk Patients Post-Catheter Ablation for Atrial Fibrillation (OCEAN) trial was launched in 2016, aiming to enrol 1572 patients 12 months after successful Catheter Ablation (no recurrences). The Investigators were only enrolling moderate or high-risk patients (at least 1 risk factor) and comparing the rates of stroke or significant blood clots over 3 years.
Unfortunately, the non-blood thinner group will all receive aspirin, so there is no ‘no treatment group’. This is a shame for patients in the UK as we don’t use aspirin after ablation anyway. It is used commonly in Canada where the study Principal Investigator is based. We know aspirin still carries a risk of bleeding and so this may neutralise the benefit of being off blood thinners have- but we will have to wait and see the results of the study.
The Investigators were making great progress with enrolment till 2020 but recruitment lowed due to the Pandemic and expect to complete enrolment now in 2025.
Summary
It is unsatisfying to not have the data to provide to patients to make this decision. And it feels like we’ve been waiting for this data for a long time. These studies need 1000s of patients to be able to make conclusions about stroke rate and studying this many patients takes time. ndeed, reflecting on this question five years later, we don’t have any strong data to point us one way or the other.
So the conclusion we drew in 2019 remains the same in 2024-
we [doctors] will have to continue to be honest and tell them [patients] that at the moment no-one knows what is correct and to do our best to help them make a decision that they are comfortable with.
References:
Our critical analysis from 2019: Ahluwalia N, Schilling R. Are there enough data to safely withdraw anticoagulation after atrial fibrillation catheter ablation? European Journal of Arrhythmia and Electrophysiology. 2019; 5(2):82–86
React-AF study design: Peigh G, Passman RS. "Pill-in-Pocket" anticoagulation for stroke prevention in atrial fibrillation. J Cardiovasc Electrophysiol. 2023 Oct;34(10):2152-2157. doi: 10.1111/jce.15866. Epub 2023 Feb 23. PMID: 36806796.
Ocean-AF study design: Verma A, Ha ACT, Kirchhof P, Hindricks G, Healey JS, Hill MD, Sharma M, Wyse DG, Champagne J, Essebag V, Wells G, Gupta D, Heidbuchel H, Sanders P, Birnie DH. The Optimal Anti-Coagulation for Enhanced-Risk Patients Post-Catheter Ablation for Atrial Fibrillation (OCEAN) trial. Am Heart J. 2018 Mar;197:124-132. doi: 10.1016/j.ahj.2017.12.007. Epub 2017 Dec 8. PMID: 29447772.
