Shortness of breath
The second most commonly reported symptom is associated with atrial fibrillation, present in up to two-thirds of patients. Limiting hobbies, commutes and even simple activities of daily living; patients with AF frequently report shortness of breath on exertion.
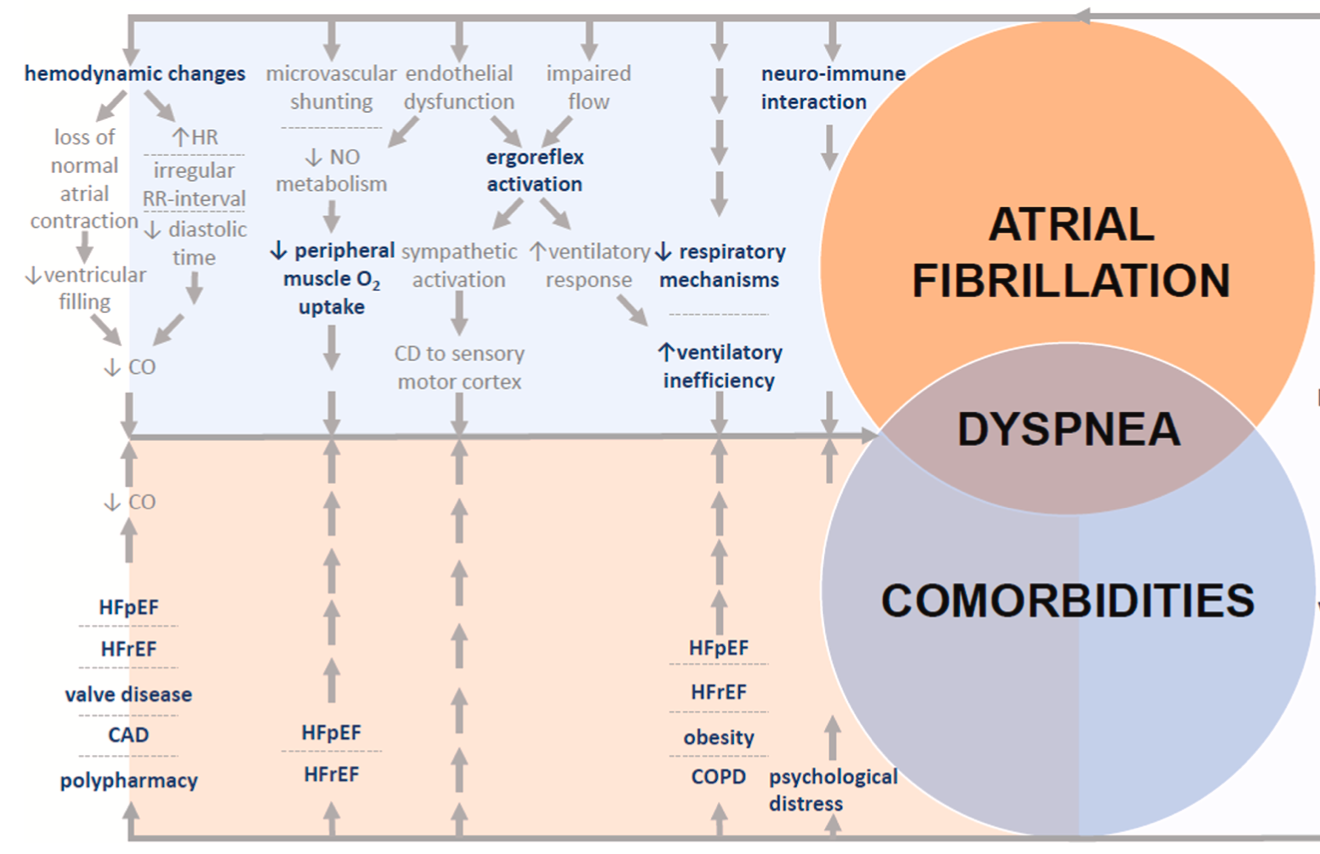
However, AF is rarely an isolated condition. Heart failure, coronary disease, muscle deconditioning, and lung disorders can frequently co-exist with AF and can all be the cause of shortness of breath. There's also a psychological element to it as well with each person's perception of 'breathlessness' being different too.
So how can we tell a patient that if we treat your AF, your breathing will get better, if we can't be sure the breathlessness is due to the AF in the first place? Let's go back to first principles and try and understand how AF can cause shortness of breath-
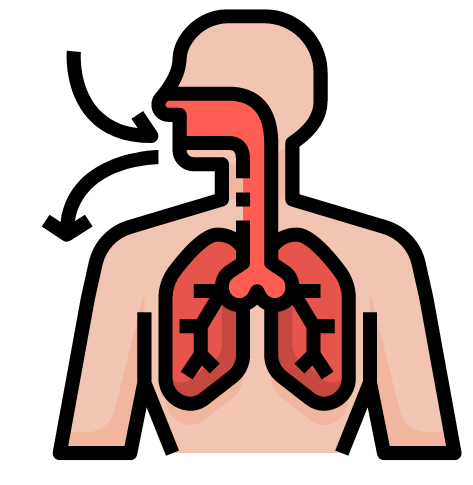
The heart is a pump responsible for squeezing blood around the body to provide the organs and muscles with the oxygen and nutrients they need. During activities, your muscles require more oxygen and nutrients but during AF, the heart can't 'step up' and increase the delivery to the levels needed. This triggers a compensatory reflex in the body to release more adrenaline and increase the blood flow and breathing rate to get more oxygen around the body.
Other mechanisms have also been suggested such as the psychological distress caused by AF triggering adrenaline release and there are also suggestions that AF causes the blood vessels in the body to react abnormally and reduce blood supply to the muscles. These reasons are explained in more detail in the paper linked at the bottom of this post.
The image below captures the complexity of the AF-shortness of breath relationship! One thing to remember is shortness of breath may sometimes be a result of the tablets you take and so it's sensible to go through these with your physician or pharmacist.
As interesting as this is, the more relevant question for patients might be "is the shortness of breath I feel due to my AF or due to something else?"
If you're AF is 'paroxysmal' (comes and goes) its more straightforward as you can compare your symptoms when you're in AF vs when you're not. If you're in 'persistent' (continuous for > 7 days), there may be a role for a trial of rhythm control e.g. a Cardioversion procedure, to see how your symptoms change when you're put back into normal rhythm (i.e. if your breathlessness is AF-driven, it should get better soon after you're back in normal rhythm). Cardio-pulmonary exercise testing has a role in challenging cases and can help detect underlying lung or other heart conditions. There are also some features on an echo (an ultrasound scan of your heart) that might suggest other cardiac causes too.
The AFHF study is trying to characterise this concept of 'AF-mediate shortness of breath' and is using comprehensive questionnaires to evaluate how the symptom changes before and after ablation. Different features are being measured to determine what differs between the patients who get better versus the patients who don't. Depending on the results, the predictive features could be used to tell future generations of patients "Your shortness of breath is likely to be due to your AF and it should get better if we treat your AF" and vice versa.
So watch this space!
van der Velden RMJ, Hermans ANL, Pluymaekers NAHA, Gawalko M, Elliott A, Hendriks JM, Franssen FME, Slats AM, van Empel VPM, Van Gelder IC, Thijssen DHJ, Eijsvogels TMH, Leue C, Crijns HJGM, Linz D, Simons SO. Dyspnea in patients with atrial fibrillation: Mechanisms, assessment and an interdisciplinary and integrated care approach. Int J Cardiol Heart Vasc. 2022 Jul 19;42:101086. doi: 10.1016/j.ijcha.2022.101086. PMID: 35873859; PMCID: PMC9304702.
