Having a second AF ablation? Here's what you need to know
"Am I having a repeat AF ablation because it wasn’t done properly the first time?"
This is highly unlikely to be the reason. Complete AF ablation treatment can require more than one procedure because there are things that cannot and should not be tackled on the first sitting- your physician should make you aware of the potential need for a repeat procedure for full benefit. Just because it’s called a repeat ablation does not mean the strategy is the same as well. We go through the common reasons for AF recurrence after ablation and potential strategies to deal with it on the second sitting.
What happened in the first procedure?
AF catheter ablation is the most effective therapy at restoring normal rhythm and reducing AF symptoms. Many patients with this condition opt for catheter ablation when medications aren't working.
The cornerstone of catheter ablation is pulmonary vein isolation- electrically blocking the pulmonary veins (the region connected to the upper left heart chamber- the site where AF ‘trigger beats’ originate from in 90% of cases).
There is little evidence for doing any ablation beyond this treatment area on the first attempt and when studied side-by-side more extensive ablation doesn’t seem to add any benefit- so the evidence says we should not go beyond this (although there is a lot of ongoing research trying to change this) . This electrical block around the pulmonary veins can be done using radio frequency (heat therapy) or cryoballoon (freezing therapy) ablation- which have shown equivalent success.
Recurrence of AF after ablation is quite common. For patients who initially have a successful procedure, between 60-80% remain free from AF a year later. But that means 20-40% might experience a recurrence. Remember your unique ‘single procedure success rate’ may vary based on your age, time in AF and risk factors (weight, high blood pressure, heart structure).
In rare cases, electrical block of the pulmonary veins isn’t possible- perhaps due to difficulties reaching the right parts of the heart, poor tolerability if done under local anaesthetic or concerns about a potential complication, but the vast majority of patients leave the AF catheter lab with electrical block of their pulmonary veins and go home in normal rhythm.
Monitoring for Recurrence
Given that AF can recur after treatment, routine follow-ups are important. Patients should typically see their doctor at least 3 months after the procedure and then every 6 months for the next two years. If you feel fluttering or irregularities in your heart rhythm during this period, it's crucial to inform your doctor. They may provide a monitor to track your heart rhythms for signs of recurring AF.
Recurrence of AF
Early recurrence of AF episodes in the blanking period can be temporary- caused by the inflammation from the ablation procedure and will settle down as the treatment beds in. This can occur in the first 6-12 weeks.
When relapse occurs after this, it is most commonly due to one of two reasons; the veins have reconnected due to a gap that has formed in the initial ablation treatment loop (allowing AF to ‘leak’ in from the pulmonary veins into the heart via this passage way or a new, non-AF arrhythmia has emerged.
Reconnected pulmonary veins
Although the ring of block can appear complete at the end of the first ablation, small gaps can emerge as sections can recover, especially once the inflammation and immediate effects of the ablation settle down. Unfortunately, predicting the long-term durability of an ablation ring can be difficult to assess at the time of the first procedure. It is standard practice to give 10-20 minutes after the ablation treatment before going back and checking it is blocked but still- things can change months down the line.
At repeat ablation, the first step is often to check the completeness of an ablation ring. If gaps are identified, these can be specifically targeted to ‘top-up’ the ablation and re-achieve block. This requires sensitive mapping tools that are able to find the gaps in the ring and as ablation mapping technologies improve the accuracy of finding these gaps get better. The hope being that better identification of gaps, means more likely to achieve complete block after a second ablation procedure and thus the long-term freedom from AF is better.
Other atrial arrhythmias
Recurrence of symptoms might not necessarily mean recurrence of AF. We know atrial flutter, an abnormal rhythm from a different part of the heart are more common in patients with AF. Other atrial arrhythmias can emerge after an AF ablation and so even in the setting of complete pulmonary vein block, arrhythmias can arise. Now developing a second arrhythmia a few months after treatment of the AF is not a coincidence. Firstly, the removal of AF may unmask other irritable areas of the heart that become dominant and emerge. Alternatively the ablation lines themselves can lead to electrical interference in the normal conduction and precipitate new arrhythmias to occur as a result of the ablation treatment. Often, these look different to AF on the ECG and your doctor may describe it as ‘more organised’. These are referred to as atrial tachycardias or AT’s. The complexity of ATs can vary significantly- meaning the repeat ablation, if it’s for an AT, could take 30 minutes or three hours. Again, the development of better mapping tools means we can track the origin sites of these ATs more easily and hopefully improve outcomes.
A strategy for repeat AF ablation
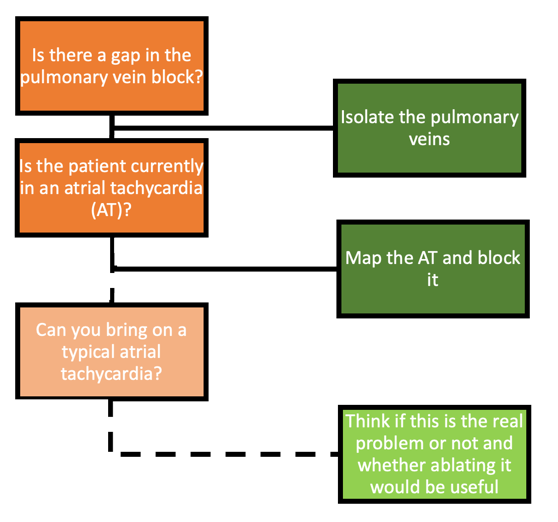
The actual strategy that an electrophysiologist will employ for a repeat procedure will be entirely personal. It will depend on what your ECGs have shown previously, the findings at the time of the first ablation procedure and what they have discussed with you.
However taking the above points into consideration, there is a basic framework that we can begin to draw up that will address the different types of arrhythmia that can occur. Whereas most electrophysiologists will tackle an AT that’s present from the start of the procedure (and seen at the time of symptoms), there is much greater uncertainty about what to do with ATs that emerge during the procedure. As we’ve said, the ablation treatments can actually precipitate future arrhythmias in some cases and so you have to be sure that treating one will result in improved symptoms. ATs that occur during an ablation procedure may simply be a result of the ablation catheters moving around inside the heart and so they may not be as important in driving symptoms and so tackling them is much harder to justify. But each patient is unique and so this is usually a judgement call taken at the time of the ablation procedure.
Conclusion
Recurring AF after catheter ablation can be disheartening, but it's important to remember that it's not uncommon, and it's certainly not the end of the road. With ongoing monitoring and a personalised treatment approach, recurrent AF can be managed effectively. Discuss any concerns you may have, and try to keep a diary of symptoms, especially in the first 6 months after ablation. And even if AF recurs after repeated ablations, there are alternative strategies that you can consider with your healthcare team.
This information is meant to provide a general overview and may not apply to everyone. Always consult with your healthcare provider for personal medical advice.
