Measuring severity of AFib
“How do you feel?”
this ambiguous question is frequently asked of people with Atrial Fibrillation during their hospital consultations or if they become unwell and present to the Emergency Department. But how should this nebulous question be answered? and does it alter the treatment decision a doctor is going to make?
Most treatment decisions and clinical research today around AFib is aimed at achieving better symptom management.
Symptom severity guides treatment
The cornerstone of AF care remains the consideration of stroke risk and the role of blood thinners. However this is usually addressed within the first consultation and, for most people, its an algorithm-guided decision. Ongoing treatment plans and interventions are driven by the goal of achieving better control of AF-related symptoms. The mantra from the business world-
What gets managed must first be measured
can be applied to this aspect of AF care too- we need a scale against which to determine if treatments are actually having the desired effect. Unfortunately, herein lies tremendous complexity.
Approximately 70% of patients experience symptoms with their AF and one American registry has reported 30% of people with AF are hospitalised per year.
Improving AF management is an ‘NHS priority’ in the NHS Long Term plan, with similar initiatives in place across Europe and America too.
We have a range of treatment options (although paradoxically it can often feel like there are not enough!) from anti-arrhythmic drugs, electrical cardioversion, ablation procedures and pacemakers. But the treatment of choice will vary by person based on their health, the characteristics of their AF and importantly by the severity of their AF symptoms. The treatment for the same individual with “asymptomatic” AF” or “mild” AF symptoms can vary from their treatment if they had “severe” AF symptoms.
What is a symptom?
But a ‘symptom’ is highly subjective and it cannot be answered in a yes/no question either.
Symptomatic AF is the main reason the procedure is done, and it is not risk-free. We need to measure the impact of symptoms on an individuals life so the individual can consider whether the risks are worth the potential benefit of symptom improvement.
So, we need a ruler to measure the severity and impact of AF.

Measuring AF symptoms
Clinical Trials and treatment evaluations have traditionally measured the “freedom from AF” as ruler of choice. For example, if we give 100 patients with AF Drug X or Procedure Y, how many of them will be free of AF in 12 months? Recently, this has evolved to measure how much time is spent in AF in the 12 months after the treatment, converting the yes/no answer into a more nuanced percentage. But if the main reason for the prescription of anti-arrhythmia drugs or undertaking the AF ablation procedure was symptom reduction, why aren’t we measuring the change in symptoms?
There is good evidence to suggest that for some people the ‘amount of AF’ is proportional to their symptom severity but that is not the case for many and why measure a surrogate if we can measure the change in symptom severity directly.
The crudest method to evaluate this is simply asking a patient:
“do you feel better?”
But this loaded question can prompt a “yes doctor” in the clinic even when it is not the case. Similarly, asking someone to rate their symptoms on a scale of 1-10 is too broad and may vary by the time of day/day of the week. A 7 out of 10 to patient 1 might be acceptable but to patient 2, represent an unbearable quality of life.
And so, validated ‘Health Related Quality of Life’ questionnaires have been developed to try and provide some nuance to this challenge. The most frequently used and validated questionnaire in AF care is the AFeQT (the Atrial Fibrillation Effect on QualiTy-of-life Questionnaire.
You can view the 22-question AFeQT survey tool here
It considers many aspects of life, such as physical symptoms, impact on daily activities, emotional impact and treatment concern.
For any participant in the AFHF or AFFU-AW study, you will be familiar with it from your pre-ablation and post-ablation appointments (sincere thanks to everyone who completed these!)
It is an imperfect tool but it aims to apply a number out of 100 to a highly subjective and multi-dimensional feeling.

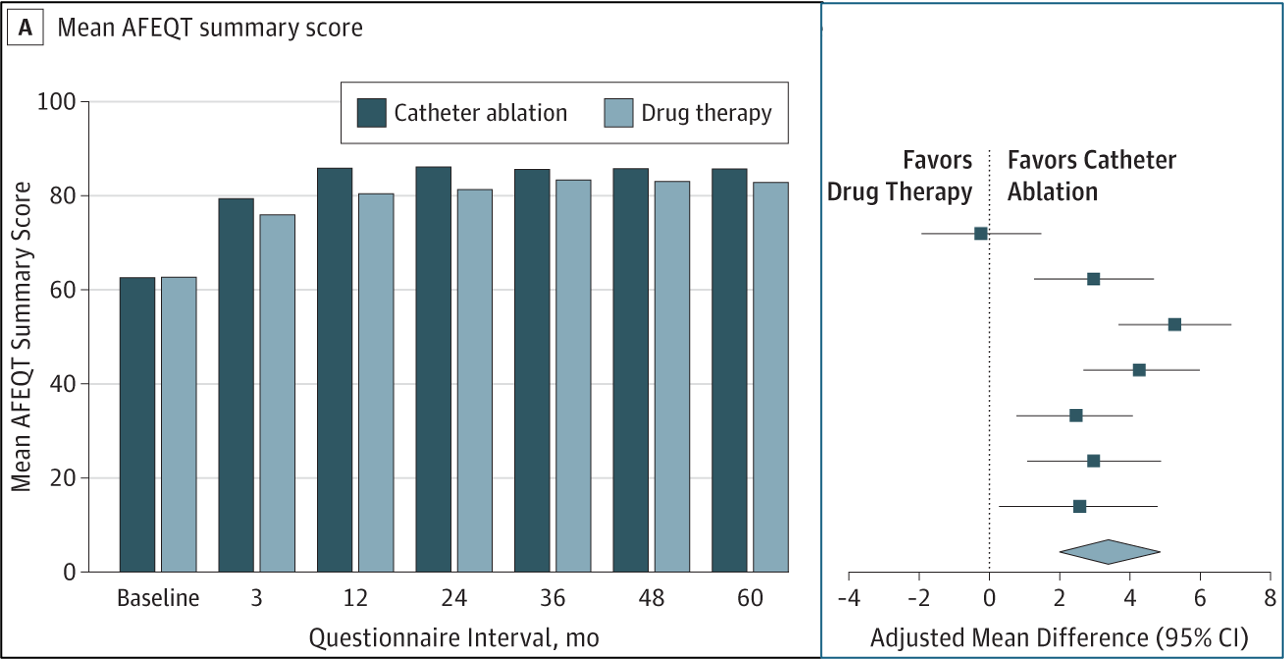
The largest Randomised Clinical Trial to use a questionnaire to measure the effect of treatments on AF symptoms was the CABANA trial. The study compared the effect of catheter ablation against medical therapies on symptom severity.
Participants in both study groups improved their symptom severity i.e. improved their AFeQT score at follow-up. Participants who received catheter ablation appeared to have a better AFeQT score i.e. greater symptom reduction although the difference between the ablation group and medication group was only 3.4 points out of 100 by final 5 year follow-up.
Can we do better?
Applying a number to symptom severity allows one to compare the effectiveness of different treatments and track patient progress over time. If we understood how AF caused symptoms then that may help us identify tests and investigations that may better track the underlying mechanism that determines symptom severity.
One of the additional objectives of the AFHF trial is trying to do that (in fact, analysing the data from our patients in this study and subsequently going down a rabbit hole of the complexity of symptom survey data analysis is what triggered this post!). We are exploring:
- how closely ’exercise capacity’ on a cardiopulmonary exercise test aligns with a person’s opinion of their own exercise capacity
- how the ‘stiffness’ and ‘pressure’ in the heart aligns with a person’s opinion of their own ‘breathlessness’

We are also reviewing differences between patients who feel their symptoms get better after AF ablation versus people who do not- although the CABANA study above shows that on average people feel better, this is not seen in all patients and we don’t know what that is.
But the reality is even if these markers correlate with symptom severity, one marker will not be able to replace a persons symptoms severity because psychosocial components play a big role too. We need to understand:
The relationship between AF and depression. (the next post coming)
The relationship between AF and socio-economics (also coming soon)
These factors will determine the relationship between objective limitations in function (i.e. what we measure on a breathing or exercise test) and the perception of symptom severity and impact on an individual patient. And ultimately that perceived impact is probably should be used to guide a person’s treatment plan, because they are the one living with the AF and taking on the risk fo any treatment options.
It is easier to measure heart function on an Echo scan or the amount of time in AF on a 24-hour ECG monitor but if AF treatments are prescribed or performed for symptom improvement, we need better ways to measure this directly.
It is important to understand how AF causes impairment of exercise capacity and breathing but this won’t replace the patient-reported measurement of AF symptoms which should remain at the core of how we assess AF treatments and technologies.
A request
Do you have any ideas? If you live with AF or who knows someone who does, it would be great to hear your thoughts and ideas on how we can better measure AF symptom severity. Please do reply to this email or get in touch at nikhil@bartsaf.com. Please forward this to anyone you think would be interested or have thoughts as it could help unlock new ideas and tools for AF research and trials. Thank you!
