Left atrial fibrosis and AF
I've referred to left atrial fibrosis in a couple of previous posts and today, I want to take a deep dive into what that actually means.
Understanding Left Atrial Fibrosis in Atrial Fibrillation Patients
Fibrosis of the heart describes the formation of excess fibrous connective tissue in the heart muscle. Fibrosis of the heart is commonly seen after heart attacks, in heart failure, in inherited heart diseases, and in atrial fibrillation. The pattern of fibrosis and extent of fibrosis is important and differences in location are seen across the various diseases. For atrial fibrillation, we think the fibrosis in the left atrium (the top left heart chamber) is the most relevant (as this is the main chamber where AF originates from). Post-mortem studies have shown a correlation between AF and the degree of atrial fibrosis and animal studies have shown that fast pacing of the atrium causes AF and atrial fibrosis as well.
However, this may be another chicken and egg scenario- does the AF cause the fibrosis, or does the fibrosis lead to the AF? One possibility is that the accumulation of fibrous tissue can disrupt normal electrical signaling, resulting in an increased risk of atrial fibrillation. In addition, fibrosis can result in maze-like electrical barriers in the heart chamber, which can cause lead to disruption of the electrical waves in the heart causing the chaotic smaller circuits that are detected during AF.
Atrial fibrosis also increases with aging, heart failure, and elite levels of exercise- so maybe fibrosis is the mechanism through which these risk factors lead to AF.
Imaging Atrial Fibrosis
Fibrosis can only be officially diagnosed by taking a sample of the heart tissue and looking at it under a microscope. So cardiologists have developed non-invasive ways to try and detect fibrosis instead.
Atrial fibrosis can be assessed using a special contrast MRI scan of the heart. This has been used for decades to visualise tissue damage after heart attacks. However, detecting fibrosis in the left atrium can be more challenging as the wall is thinner and harder to see in the presence of AF when the atrium is moving faster.
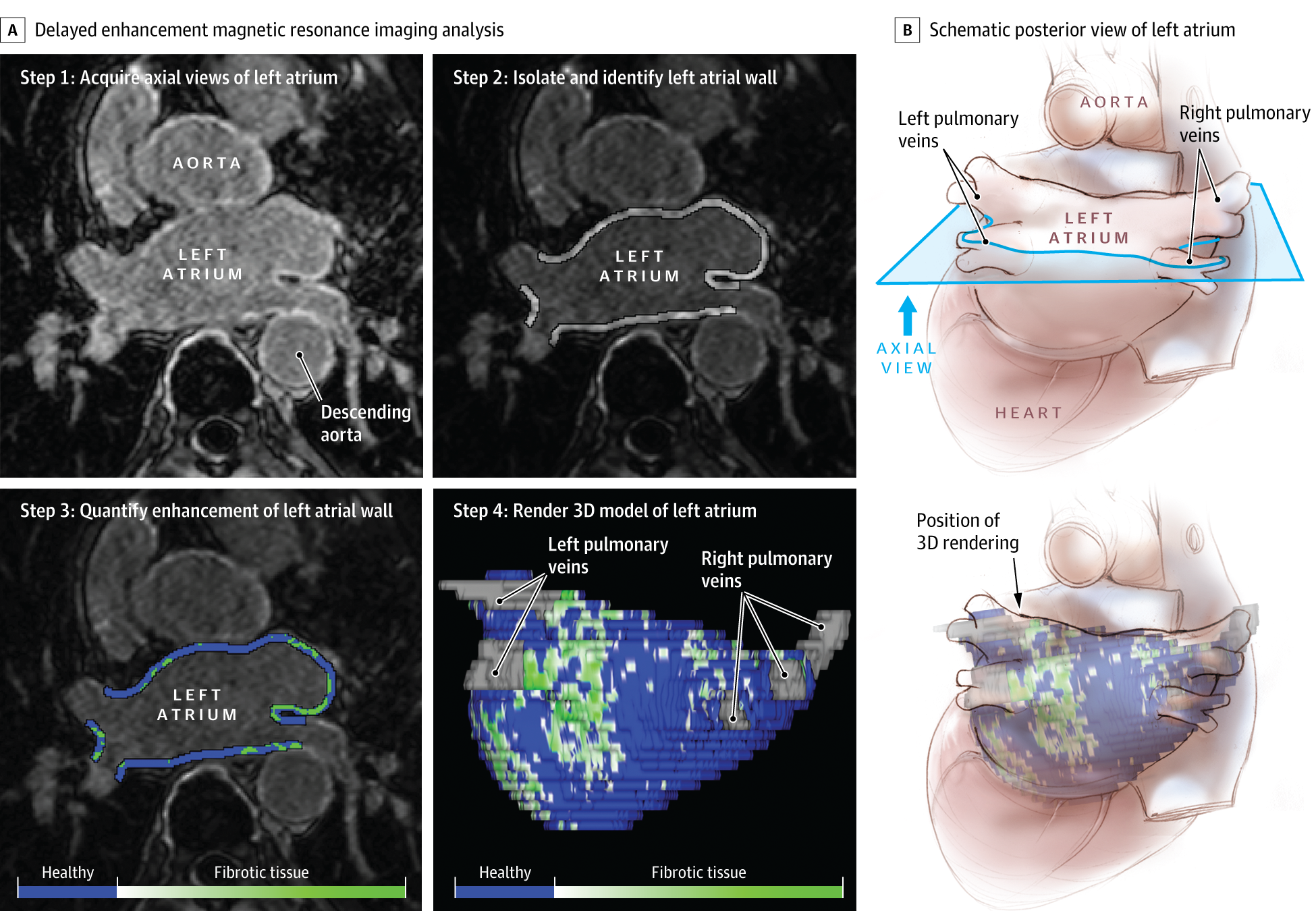
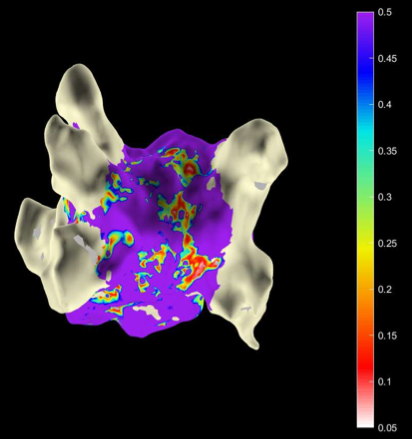
Another approach is to look for areas of poor electrical conduction during an ablation procedure. We know that fibrotic areas conduct electrical current poorly and so we think that ‘low voltage zones’ that can be detected with ‘mapping catheters’ might identify areas of fibrosis. For those of you who have had an ‘RF’ ablation or ‘RadioFrequency’ ablation, you may have seen the colourful map that your Electrophysiologist is mapping out. The colours can be set to represent areas of different voltage levels and although each ablation manufacturer will use different settings, often red or grey areas are used to suggest ‘low voltage zones’
Does it affect the management of AF?
Again, this is a relatively new area in cardiology and so it is important to distinguish between the evidence and what we think it could mean. Some centres that can measure atrial fibrosis on MRI have reported that it is a good predictor of poor outcomes from ablation- i.e. people with lots of fibrosis are less likely to stay in normal rhythm. This makes sense in that more fibrosis may suggest more entrenched AF that is harder to reverse and eliminate.
But studies targeting these areas of fibrosis with extra ablation have shown mixed results. The largest study to date compared MRI-guided fibrosis ablation + standard ablation versus standard ablation alone and failed to show any significant benefit. However, a smaller study targeting the areas of low voltage seen during the ablation mapping has suggested there may be an improvement in freedom from AF when this approach is added on top of standard care. Before exploring this further, we need a better understanding of how to assess fibrosis with these technologies reliably and also which types of patients are likely to benefit the most from paying attention to their atrial fibrosis patterns.
Marrouche NF, Wilber D, Hindricks G, Jais P, Akoum N, Marchlinski F, Kholmovski E, Burgon N, Hu N, Mont L, Deneke T, Duytschaever M, Neumann T, Mansour M, Mahnkopf C, Herweg B, Daoud E, Wissner E, Bansmann P, Brachmann J. Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation: the DECAAF study. JAMA. 2014 Feb 5;311(5):498-506. doi: 10.1001/jama.2014.3. Erratum in: JAMA. 2014 Nov 5;312(17):1805. PMID: 24496537.
Marrouche NF, Wazni O, McGann C, Greene T, Dean JM, Dagher L, Kholmovski E, Mansour M, Marchlinski F, Wilber D, Hindricks G, Mahnkopf C, Wells D, Jais P, Sanders P, Brachmann J, Bax JJ, Morrison-de Boer L, Deneke T, Calkins H, Sohns C, Akoum N; DECAAF II Investigators. Effect of MRI-Guided Fibrosis Ablation vs Conventional Catheter Ablation on Atrial Arrhythmia Recurrence in Patients With Persistent Atrial Fibrillation: The DECAAF II Randomized Clinical Trial. JAMA. 2022 Jun 21;327(23):2296-2305. doi: 10.1001/jama.2022.8831. PMID: 35727277; PMCID: PMC9214588.
Huo Y, Gaspar T, Schönbauer R, et al. Low-Voltage Myocardium-Guided Ablation Trial of Persistent Atrial Fibrillation. Nejm Évid 2022;1(11).
