Extra heart beats after ablation
"The ablation worked but I'm still feeling very brief symptoms that are different from my AF."
The primary indication for catheter ablation for Atrial Fibrillation is to improve symptoms from the arrhythmia. The most common symptoms of AF are palpitations and shortness of breath and after a successful ablation, many patients do report an improvement in symptoms.
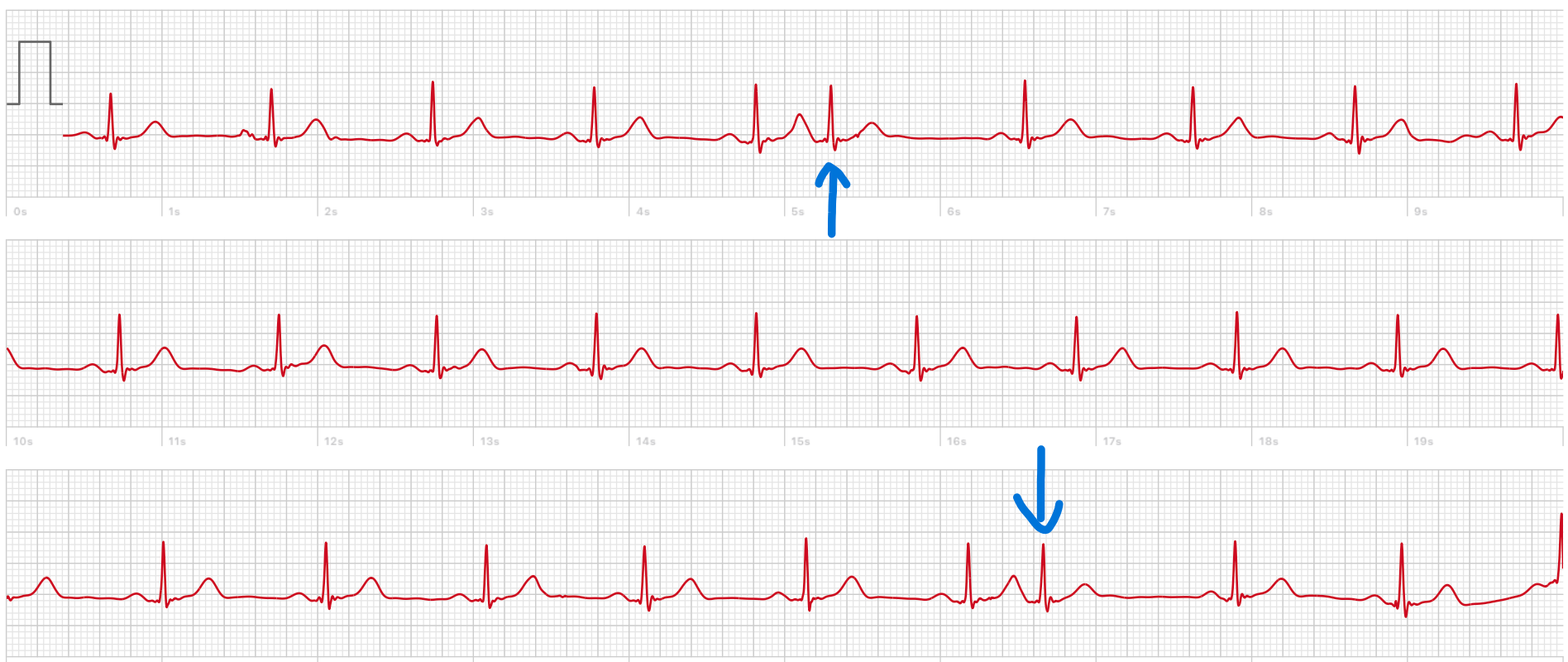
On occasion however at the 3-month post-ablation appointment patients may say “I get a different type of palpitation, lasting only for a few seconds”. These very short symptom episodes can be really challenging to capture on a traditional ECG. Although it could be AF, this is less likely. More commonly, very short episodes like this are due to ectopic beats. Detecting this is important because their management and prognosis is very different from AF.
Ectopic beats after Catheter Ablation can lead to much anxiety, especially if you never had these symptoms before ablation.
What is an ectopic beat?
Normal heartbeats originate from the same point of the heart- the sinus node. This collection of specialist cells generate the electrical impulses that cause the heart to beat in an orderly manner.
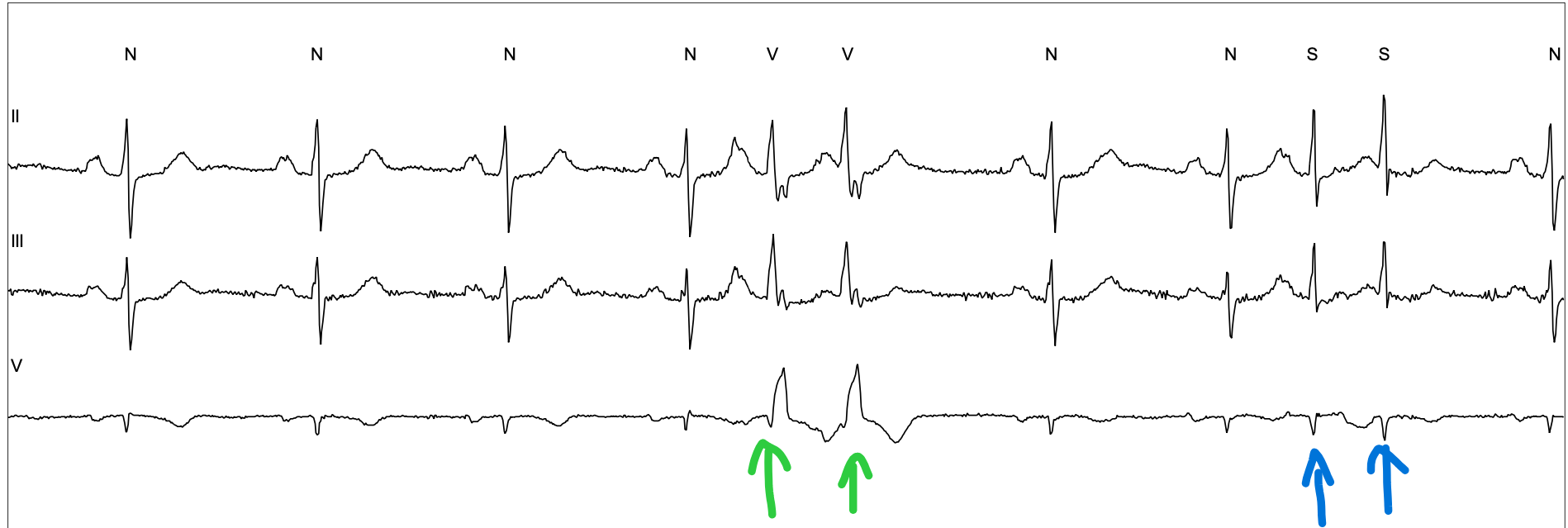
Ectopic heart beats prematurely originate from other parts of the heart and take over the heart beat. These can occur in isolation- with normal sinus rhythm immediately restored, or in short runs of a few in a row. Patients can describe the sensation of feeling winded or can’t get enough air in or even butterflies in their stomach like they’re going down a rollercoaster. Ectopic beats are very common in the population. Any heart tissue has the potential to trigger an ectopic and so the occasional rare ectopic is not abnormal. When these originate from the bottom chamber of the heart they are called ‘Ventricular ectopics’ and when they originalte from the top chambers of the heart, they are called ’Supra-ventricular ectopics’
Supra-ventricular ectopic heartbeats can be the trigger for AF episodes before the ablation. The most common ablation technique is ‘pulmonary vein isolation’ which is designed to block the ectopic heartbeats from entering the heart from the pulmonary veins that initiate AF. After an ablation, patients may simply be more aware of their heart beat because of concern that AF may recur. So patients who notice ectopic beats after their ablation may simply notice symptoms that they would not have been consciously aware of in the past.
How common are ectopic beats after ablation?
As we have said, ectopic beats are very common in the general population and are often the trigger for AF. Although pulmonary vein isolation can be effective in blocking the ectopic beats from the pulmonary veins, it can take a few weeks for the ablation lesions to fully form. Therefore ectopics from the veins may still be seen immediately after the ablation and ectopics from other sites can still occur at any time.
It is so common that we don’t normally measure the amount of ectopics routinely after ablation. One study that of 125 patients after their first AF ablation who fitted with a 7-day monitor after their ablation showed ectopics in most patients too. The amount of ectopics varied from less than 72 beats/day in the lowest 25% and more than 783 beats/day in the highest 25%. We don’t know why this happens, one study that took blood samples showed an association between markers of inflammation and ectopic beat burden- so it may be due to the inflammation caused by the ablation treatment itself.
In the AFFU-AW study- where we are routinely monitoring the heart rhythm once per day using the Apple Watch, we are seeing some ectopic beats in many patients, probably more than half (this is an estimate so don’t quote me!) one advantage we are seeing is the efficiency with which we can diagnose ectopic beats and reassure patients that their symptoms are not due to AF coming back. The automated algorithms of Wearable ECGs or Blood Pressure-based heart rate detection software is their relative inability to differentiate ectopic beats from AF. The algorithm sees an irregular heart beat pattern and errs on the side of caution, labelling it as AF which can exacerbate anxieties.

Do ectopics mean my AF will come back?
Just because you have ectopics after your ablation, does not automatically mean you will get an AF recurrence.
However, the studies that have observed patients after ablation show that patients with ectopics do have a higher risk of AF recurrence.
The study of 125 patients above showed that the number of ectopics in the 7 days after ablation was associated with the risk of AF episodes in the short-term and long-term. This relationship was dose-dependent- the more ectopics, the higher the risk.
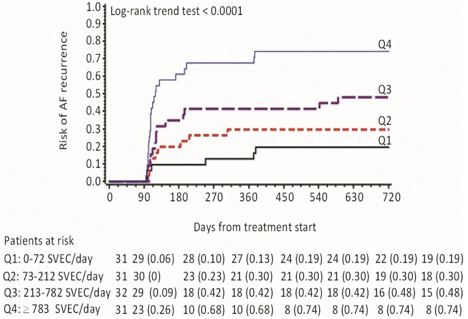
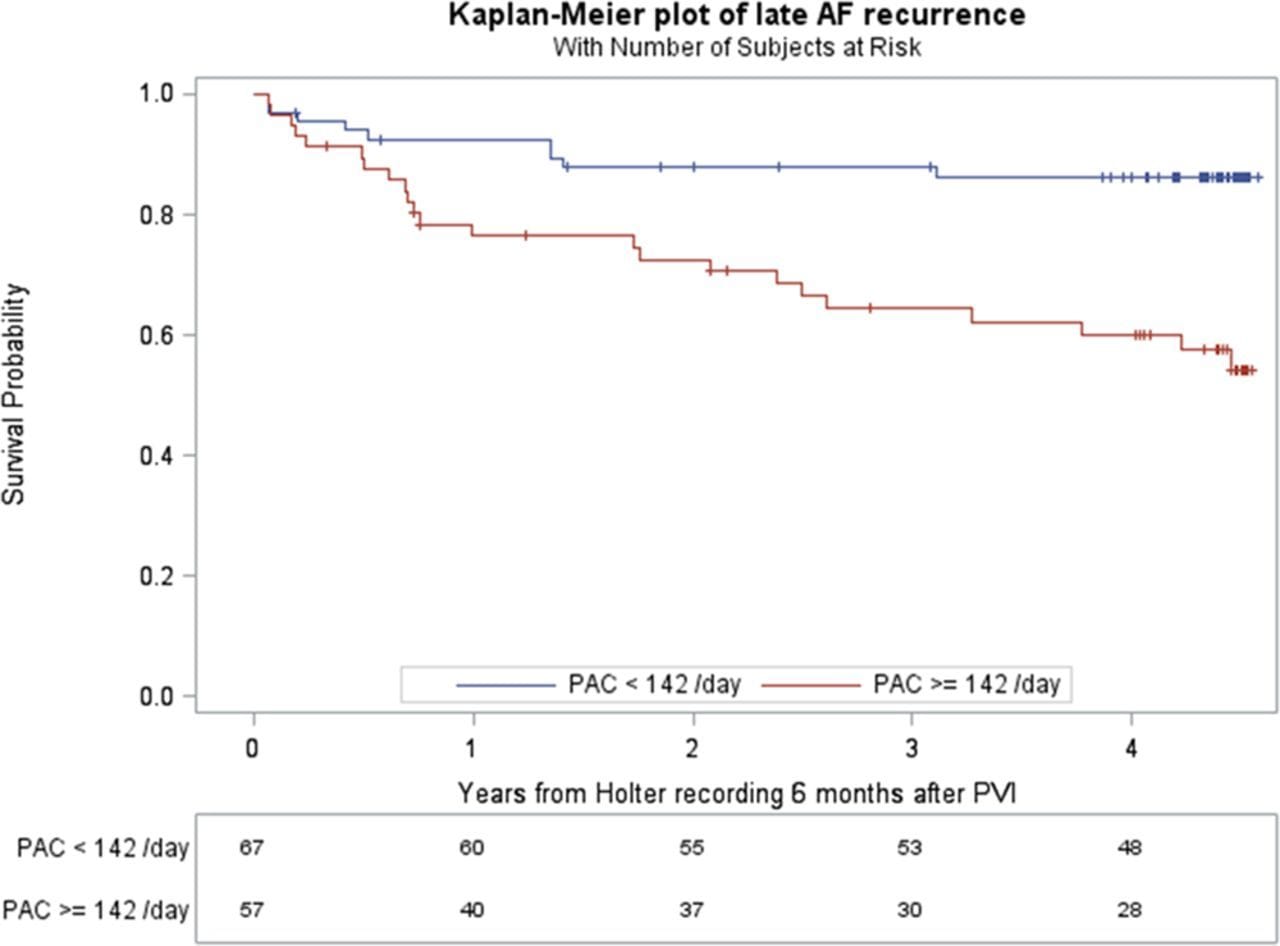
This relationship persists later into the post-ablation period. The number of ectopics at 6 months post-ablation was a predictor of late AF recurrence.
Do I need treatment for these?
In most cases, ectopics settle down spontaneously. Ectopics that occur after the ablation may settle down as the ablation treatment settles in and as recovery continues. The medications that patients take before ablation for their AF suppression (like bisoprolol, sotalol, flecainide or amiodarone) also suppress ectopics. So as these tablets are discontinued, you may notice ectopic beats after this happens.
Which begs the question, should I restart my tablets, or if not on them before the ablation- should I start some?
This may be appropriate but needs consideration:
- Supra-ventricular ectopic beats in themselves are not harmful. They are not associated with heart failure, or blood clot formation and suppressing them has not been shown to effect the stroke risk. Ventricular ectopic beats have been rarely associated with heart failure- but you need a huge number- around 20% for many months before this becomes a consideration.
- Especially in the post-ablation phase, ectopics may settle down spontaenously. There can also be an exacerbating factor like stress, infection or poor sleep that, once addressed, leads to resolution of the ectopic beats.
- Some patients may pursue ablation to try and come off their anti-arrhythmic medications. In which case continuing them out of anxiety of AF recurrence is counter-productive. If the symptoms are tolerable, it can be worth seeing how things progress off the tablets. If AF does recur, then the conversation about medications can be re-visited but pre-emptive medications may just confuse the situation.
- If you experience symptoms from the ectopics and understand the above three considerations, taking a tablet to suppress your ectopics and reduce the symptoms is a reasonable option. Before doing so, it is worth getting a period of rhythm monitoring done to evaluate your ectopic burden and confirm your symptoms align with the ectopics and that it isn’t due to something else.
Ectopics immediately after ablation and AF risk: Alhede C, Johannessen A, Dixen U, Jensen JS, Raatikainen P, Hindricks G, Walfridsson H, Kongstad O, Pehrson S, Englund A, Hartikainen J, Hansen PS, Nielsen JC, Jons C. Higher burden of supraventricular ectopic complexes early after catheter ablation for atrial fibrillation is associated with increased risk of recurrent atrial fibrillation. Europace. 2018 Jan 1;20(1):50-57. doi: 10.1093/europace/euw329. PMID: 28011799.
Late ectopics and long-term AF risk: Gang UJ, Nalliah CJ, Lim TW, Thiagalingam A, Kovoor P, Ross DL, Thomas SP. Atrial ectopy predicts late recurrence of atrial fibrillation after pulmonary vein isolation. Circ Arrhythm Electrophysiol. 2015 Jun;8(3):569-74. doi: 10.1161/CIRCEP.114.002052. Epub 2015 Apr 22. PMID: 25904494.
