First-line AF ablation
This has been one of the hottest topics in AF research in 2021/22.
There are many different ways to manage AF and the decision about which therapy to pursue first is individual- made between the patient and their medical team. Nonetheless, there is universal agreement that lifestyle changes such as regular exercise, weight management, stress/alcohol limitation and controlling risk factors like high blood pressure are essential steps to take from the very start.
Now with regards to 'rhythm control therapies' (methods to restore normal rhythm), broadly speaking, the International guidelines recommend ablation can be considered after a patient has considered medical therapies i.e. failed or not-tolerated anti-arrhythmic drugs. These medications have been around for decades and their effectiveness and risks are well known. Ablation however is a newer 'rhythm control' therapy and so the value of ablation as the first-line therapy had not been studied- until 2021.

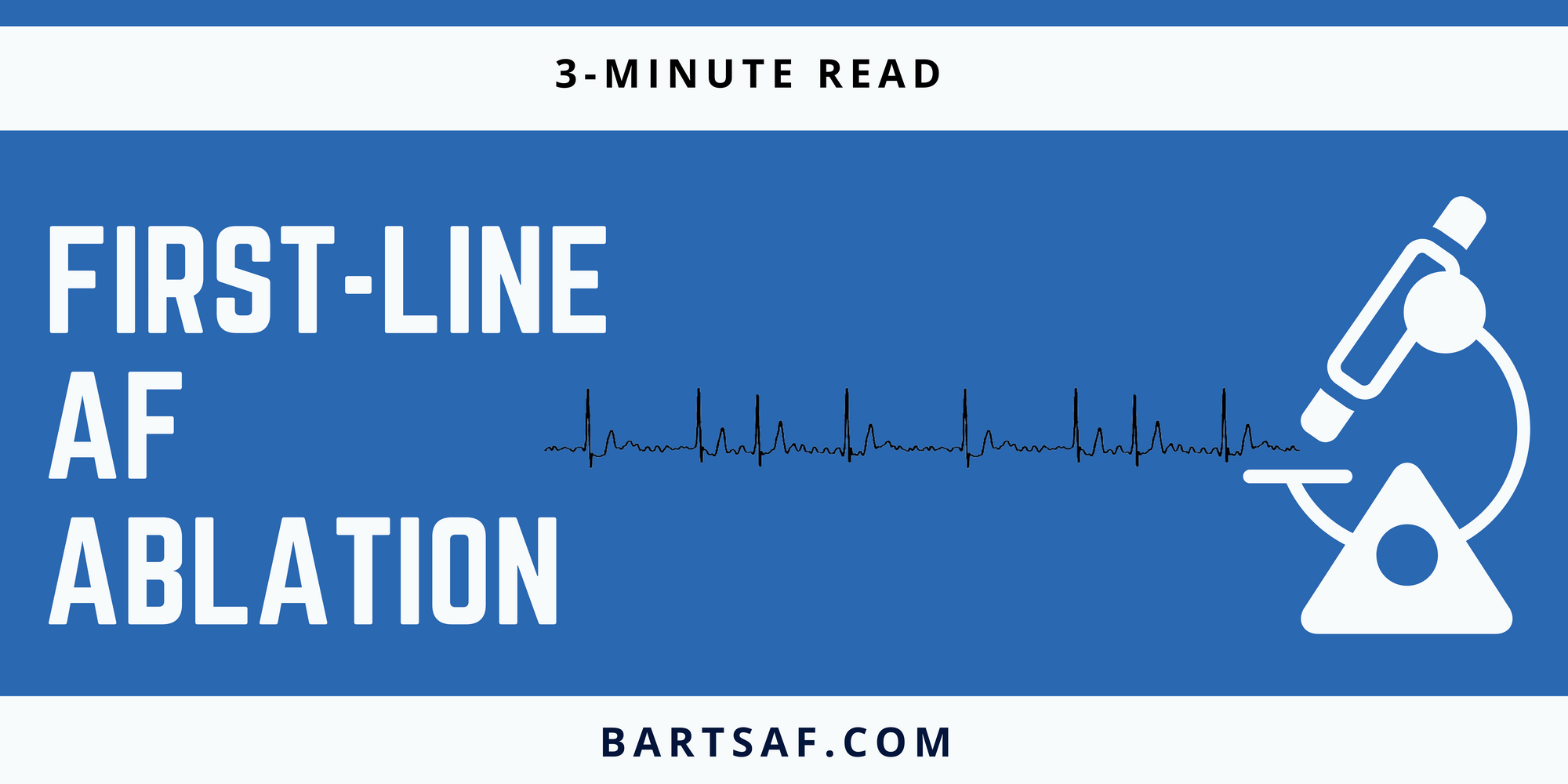
Two large multi-centre studies independently compared anti-arrhythmic drugs versus catheter ablation in treatment-naive patients i.e. as their first rhythm control treatment option. EARLY-AF was done in Canadian centres and STOP-AF in US centres.
Both studies showed a significantly lower proportion of patients who remained free of AF at 12 months after their ablation. This finding was especially robust in EARLY-AF which used implantable heart rhythm monitors for continuous monitoring throughout the follow-up period.
In summary- amongst patients receiving initial treatment for symptomatic, paroxysmal AF, ablation was superior to antiarrhythmic drug therapy for the prevention of atrial arrhythmia recurrence in patients who had not previously received antiarrhythmic drug therapies.
Some important caveats to note:
These patients were all symptomatic paroxysmal AF. We don't know how these findings relate to patients with persistent AF.
The follow-up period was only 12 months. Long-term follow-up remains to be seen.
These studies were not able to detect any significant differences in hard endpoints like hospitalisation or death.
Both studies used cryoablation as the index technique.
Similar findings were also reported in a European multi-centre study; Cryo-FIRST which adds to the weight of data on this topic

The implication of these findings is still being considered. Revised versions of the guidelines taking these findings into account have not yet been published but it is useful for patients and their physicians to be aware of these findings. As the long-term data emerges and we better understand the impact of first-line ablation on harder outcomes and survival, we'll better be able to interpret these findings in the real world.
Wazni OM, Dandamudi G, Sood N, Hoyt R, Tyler J, Durrani S, Niebauer M, Makati K, Halperin B, Gauri A, Morales G, Shao M, Cerkvenik J, Kaplon RE, Nissen SE; STOP AF First Trial Investigators. Cryoballoon Ablation as Initial Therapy for Atrial Fibrillation. N Engl J Med. 2021 Jan 28;384(4):316-324. doi: 10.1056/NEJMoa2029554. Epub 2020 Nov 16. PMID: 33197158.
Andrade JG, Wells GA, Deyell MW, Bennett M, Essebag V, Champagne J, Roux JF, Yung D, Skanes A, Khaykin Y, Morillo C, Jolly U, Novak P, Lockwood E, Amit G, Angaran P, Sapp J, Wardell S, Lauck S, Macle L, Verma A; EARLY-AF Investigators. Cryoablation or Drug Therapy for Initial Treatment of Atrial Fibrillation. N Engl J Med. 2021 Jan 28;384(4):305-315. doi: 10.1056/NEJMoa2029980. Epub 2020 Nov 16. PMID: 33197159.
