Covid and Atrial Fibrillation
“My AF only started after I got Covid. I was fine before that.”
This has not been an uncommon statement from patients with Atrial Fibrillation (AF) when they first present to Clinic. I haven’t dwelled on it too long- partly because it doesn’t change the subsequent approach to AF treatment and partly because we haven’t had enough strong data to be able to contribute anything evidence-based.
The issue is correlation versus causation-
We know Covid more commonly led to symptoms and hospitalisation in the elderly and with cardiovascular risk factors so could we clearly say that Covid caused the AF or was it simply that those patients were more likely to get AF due to the shared risk factors? To attribute causation, you want to try and understand the mechanism, i.e. explain why Covid would cause an increased likelihood of AF.
Covid is such a polarising topic online and so have not written about it previously, despite it being a clear knowledge gap for many patients and healthcare providers. But I think we now have enough good data to be able to draw some conclusions.
I have reviewed the peer-reviewed (scientifically scrutinised by other researchers) literature published in reputable AF journals and the TL;DR (Summary) is:
- If you have known AF and you develop Covid, your chances of having a major cardiovascular event (like heart failure, or heart attack) are higher than if you did not have AF.
- Whilst you have Covid, there is an increased risk of developing new AF.
- Two potential mechanisms are:
- inflammation of the heart caused by the body’s immune reaction to the Covid infection (myocarditis)
- increased stress on the heart during the infection.
- There is a much smaller, but detected, risk of AF associated with the Covid vaccine. However, vaccinated patients have a lower risk of developing AF if they go on to have a Covid hospitalisation
If you have known AF and you develop Covid, your chances of having a major cardiovascular event are higher.
This is probably unsurprising. We know that AF increases your risk of these events and so compounding two risks on top of each other is understandably going to increase your risk of a vascular event.
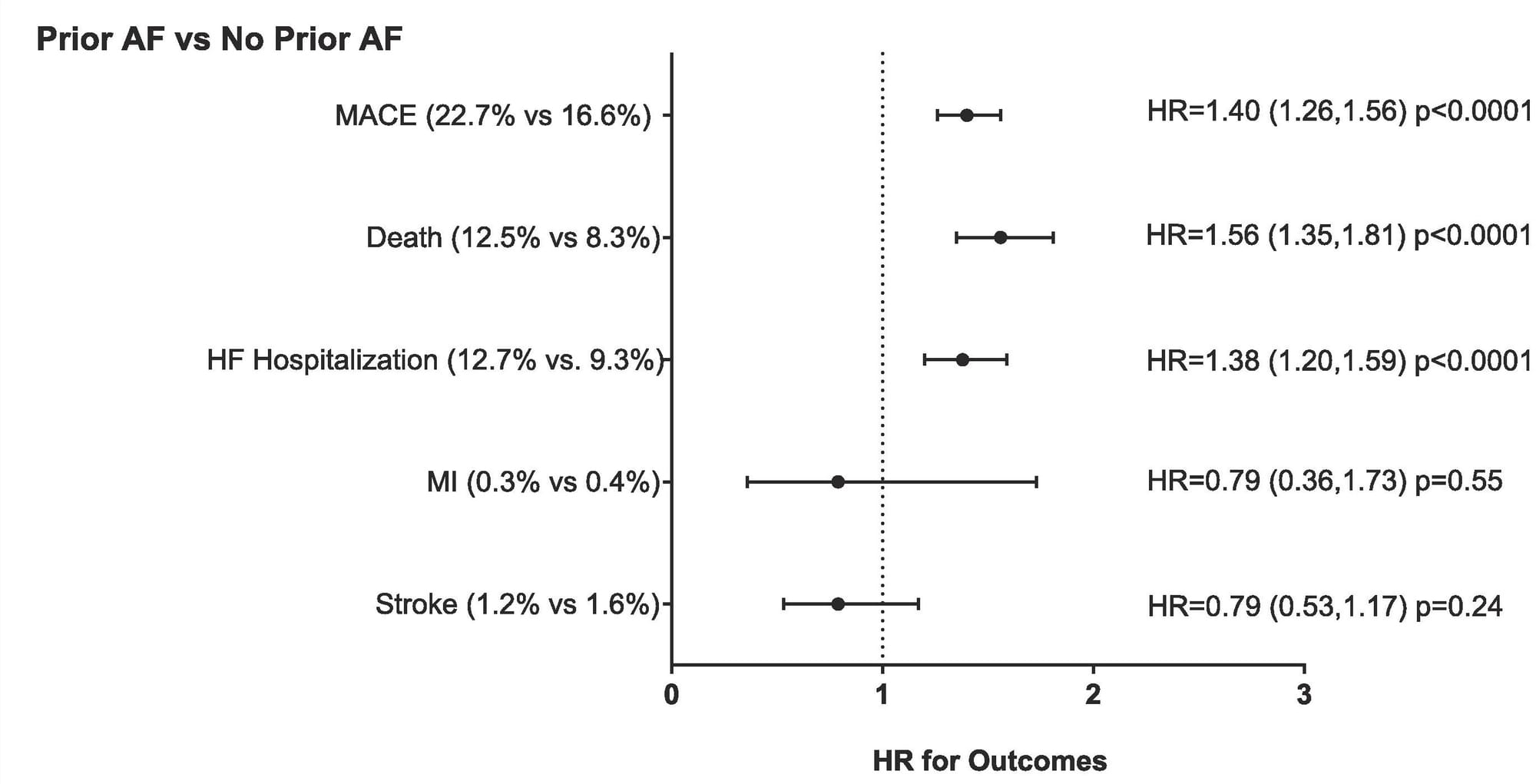
American researchers from the Intermountain Region (known for having a well-networked patient electronic health record system) matched 3623 patients with known AF who had a Covid+ test in 2020-2021 to an equivalent group of patients with a Covid+ test but no known prior AF. Patients with prior AF had a higher risk of Major Adverse Cardiovascular Events compared to non-AF (22.7% vs 16.6%). The main event type that drove this was increases in risk of Heart Failure and Death. An important sub-finding was that if you excluded the patients who had an acute episode of AF during their Covid+ period, the risk was still higher for patients with a known history of previous AF even if it wasn’t triggered during the Covid episode. The Cardiovascular event risk was lowered in patients who had been previously treated with Catheter Ablation.
If you are have severe Covid (needing hospitalisation), there is an increased risk of developing new AF- around 5%.
Several groups have evaluated this but the largest analysis was reported from the American Heart Association COVID-19 Cardiovascular Disease Registry of 30,999 patients from 120 institutions across the United States hospitalised with COVID-19. 27851 (89%) patients had no known history of AF and 1517 (5.4%) developed new-onset AF during their hospitalisation. Of patients admitted to the ICU, 12% (978/8232) had developed new AF.
At first analysis, it looked like these patients were also at an increased risk of Major Adverse Cardiac Events, like the patients with previous AF. However, on correction for their baseline risk, this relationship was no longer seen. Meaning that the patients who developed new AF were more likely to have cardiac events due to their other risk factors, regardless of whether they developed the AF or not.
A 5.4% absolute risk is quite high, but note this was amongst patients admitted in the first 2 years of the pandemic. A group from Harvard found that amongst their patients, the risk of new onset AF was 20% higher than matched patients admitted with a non-Covid diagnosis and 60% higher than in patients admitted prior to the pandemic.
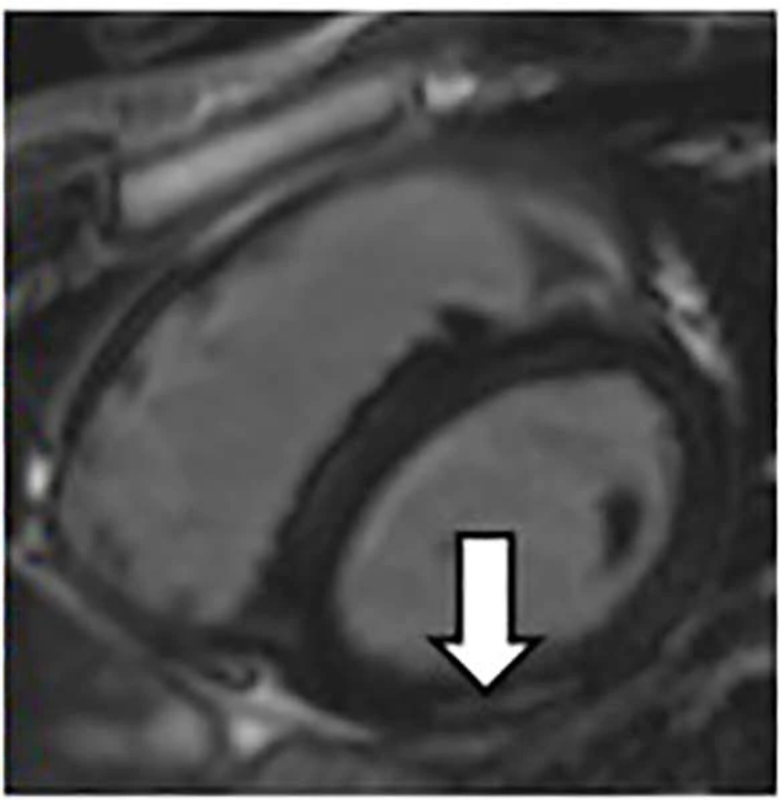
Covid and inflammation of the Heart
Researchers based at Glasgow University, UK reported their findings from 159 patients in Scotland who survived Covid hospitalisation and were invited back for a Cardiac MRI scan 2-3 months later. 1 in 8 (13%) patients were diagnosed with inflammation of the heart muscle (myocarditis), visible months after discharge home. It was ‘probable’ in a further 41% of patients based on the MRIs. Again, these findings were before the release and uptake of the Covid vaccine. Myocarditis is not unique to Covid and has been described as an after-effect of other viral illnesses too. However, we know it is a risk factor that can cause AF and may be a potential explanation for the association between Covid and AF onset. Initially, it was proposed that Covid may be directly affecting the heart muscle to cause the inflammation. However, further evaluation of the immune response to Covid suggests the inflammation may be mediated by the body's response to the virus through chemical secretions and antibodies.
Covid Vaccine and AF risk
As well as after Covid infection, a few patients have also reported their AF symptoms started the days after Vaccine dose 1 or 2. Although they have been adamant about the association, I would respond with there being no published data that I had read to be able to explain whether this was a link or coincidence. A vaccine provides immunity by precipitating an immune response to a component of the virus so the immune-myocarditis mechanism could be extrapolated, but I have not seen any mechanistic data that demonstrates this.
However, when a vaccine is first licensed, National surveillance programmes are set up around them to monitor for any possible side effects. In the UK, this is overseen by the Medicines and Healthcare products Regulatory Agency. A Freedom of Information request was submitted in 2022 asking about the reporting rates of AF after vaccination. 665 AF episodes were reported (although the time lag between vaccine and episode was not reported). This should be taken in the context of 138,785,770 doses having been administered by that time or 0.0004%. The reported incidence of a new AF episode in the Vaccine Adverse Event Reporting System limited to the Moderna vaccine in the USA was also low (23/14693) at 0.16%.
A meta-analysis (a combined analysis of all published reports) was undertaken to compare the risk of arrhythmias (abnormal heart rhythms) following Covid vaccination vs Vaccination for any other disease. incorporating 43 studies and a total of 1.5 billion vaccine doses. The reported risk of AF after Covid vaccination was higher than other vaccines but still incredibly low (3790 vs 13 cases per million doses; p<0·001). This type of analysis needs to be taken with a grain of salt as the reporting systems and data collection methodology are far more advanced during the period of Covid vaccination versus the introductory periods of other vaccines that are also administered to children who would not be at risk of AF.
Conclusion
The primary purpose of this post was to recognise the association between Covid-19 infection and AF risk. Both the risk of developing new AF and the risk of events in patients who have known AF. The data supports this relationship so for patients reporting a temporal (time-based) relationship between the two, they may likely be connected and inflammation of the heart could be one potential driver. For patients who report AF onset after vaccination, again the risk is very very low but this may well be the case. You are not being paranoid and the data has been openly published. The risk of AF is far lower after Covid vaccination than Covid infection, as well as from the other net benefits of reduced risk of severe Covid.
However, I want to reiterate my opening sentence, the focus of clinical consultation should be management and if indicated, treatment. During an acute AF episode whilst Covid +, the AF should be managed in the same way as if there was no infection (as well as treatment for Covid if indicated). Many of the AF episodes in the Vaccine reporting systems spontaneously settled down, reflecting a temporary inflammatory state that settles down with the AF abating when it does. If the AF persists, it should still be managed based on symptoms and other risk factors.
References
Rosenblatt AG, Ayers CR, Rao A, Howell SJ, Hendren NS, Zadikany RH, Ebinger JE, Daniels JD, Link MS, de Lemos JA, Das SR. New-Onset Atrial Fibrillation in Patients Hospitalized With COVID-19: Results From the American Heart Association COVID-19 Cardiovascular Registry. Circ Arrhythm Electrophysiol. 2022 May;15(5):e010666. doi: 10.1161/CIRCEP.121.010666. Epub 2022 Apr 27. PMID: 35475654.
Kumar A, Shariff M, Bhat V, DeSimone C, Deshmukh A. Atrial fibrillation after vaccination for COVID-19: analysis of the vaccine adverse event reporting system. J Interv Card Electrophysiol. 2022 Oct;65(1):1-2. doi: 10.1007/s10840-022-01263-4. Epub 2022 Jun 8. PMID: 35674855; PMCID: PMC9175153.
Silva LS, Boldrini VO, Marques AM, Yasuda CL. Post-COVID myocarditis with antiheart antibodies persistence: Clues for autoimmunity? Clin Cardiol. 2023 Mar;46(3):350-351. doi: 10.1002/clc.23979. Epub 2023 Jan 24. PMID: 36691992; PMCID: PMC10018105.
