Choosing the right rate-control drug
Learn about the different rate-control drugs available to manage atrial fibrillation, including beta-blockers, calcium channel blockers, and digoxin. Discover the latest evidence from the RATE-AF study and find out which drug might be the best choice for different patient groups.

Is there a first choice rate-control drug that patients should start with?
Comparing bisoprolol to digoxin in heart failure patients and permanent AF
Why are beta-blockers more commonly prescribed in AF?
I wrote last week about the rationale for rate control and the evidence for a possible rate threshold to aim for. However, I didn’t go into much detail about which drug to use to achieve this. In the RACE II study I discussed, the investigators allowed physicians to choose between the rate control agents I listed at their own discretion; beta-blockers, calcium channel blockers, or digoxin.
But is there a first choice rate-control drug that patients should start with?
Or are they all equal? Most AF patients can tolerate these drugs well, however, the first caveat is that there will be some patient groups where one drug is clearly not recommended due to a predisposing medical issue. For example, you would avoid calcium channel blockers in heart failure patients, avoid beta-blockers in severe asthmatics and avoid digoxin in patients with {}. But as said, for most patients, the choice is often up to the discretion of their physician and so any evidence available could help to guide this frequently encountered decision-making scenario.
A lot of the comparative work to evaluate these drugs comes out of Birmingham in the UK. The cardiology researchers there have really done some innovative studies in this area. For example, in 2020, the team published the RATE-AF study; a randomised trial comparing bisoprolol to digoxin in heart failure patients and permanent AF (remember what we said about this last week?). The study enrolled 160 patients and measured many different parameters to compare including symptom severity, quality of life, heart rate, how far a patient can walk, and heart function on echo (ultrasound of the heart). The headline result was that there was no significant difference in the impact of bisoprolol versus digoxin on symptoms (please see their beautiful results diagram below!)
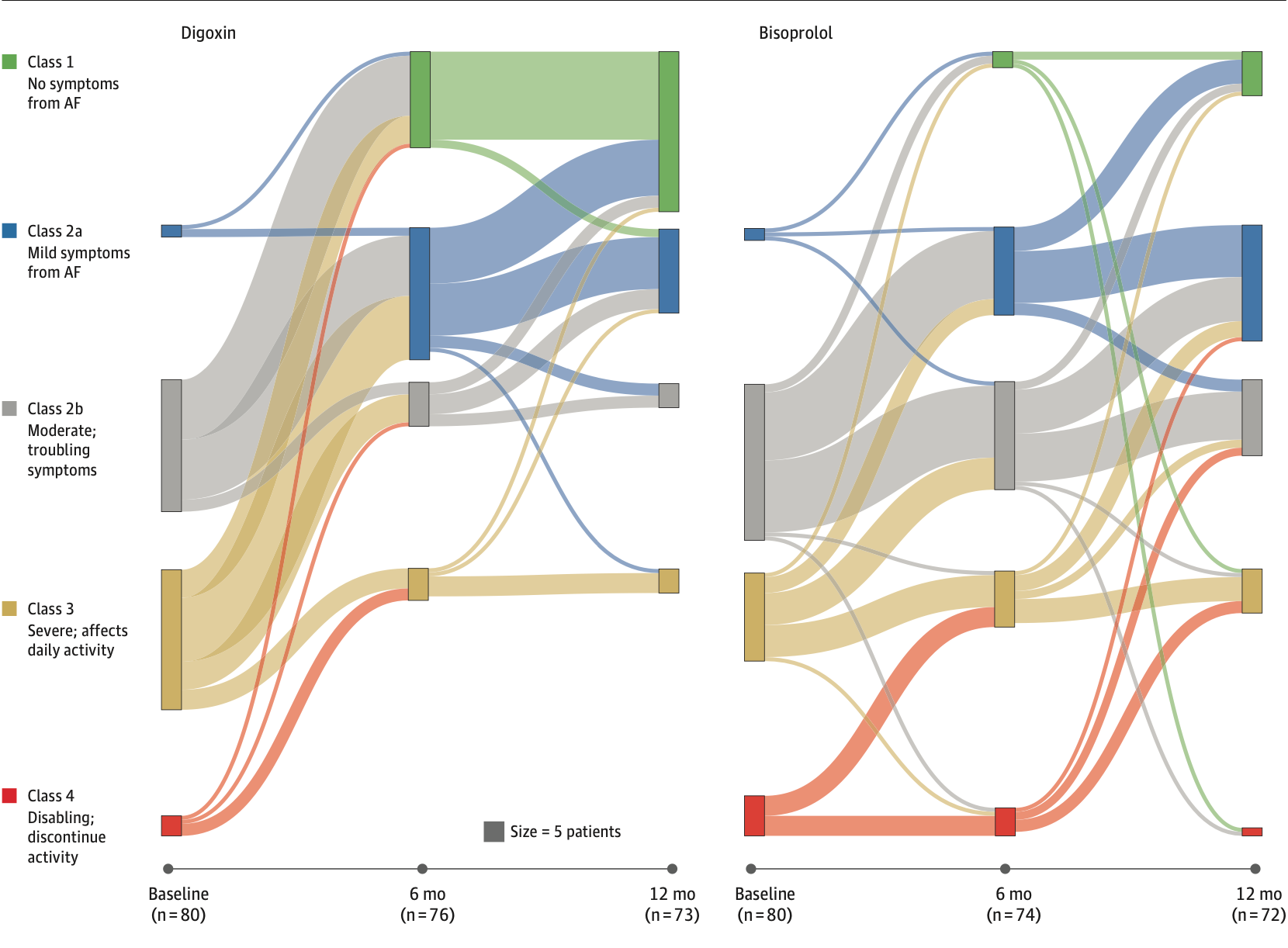
However, the authors described that more patients on bisoprolol experienced drug-related side effects, mainly excessive slowing of the heart rate with pauses and related symptoms. And so to a neutral reader, based on this information, using digoxin as the first-line drug to try would seem reasonable. However, in practice, bisoprolol is much more commonly prescribed. Why is this?
I have three possible explanations for why then beta-blockers are more commonly prescribed in AF:
- Beta-blockers have been shown to have benefits across many other cardiac diseases- hypertrophic cardiomyopathy, angina, after heart attacks and so if a patient has any of these concurrent diagnoses, prescribing a beta-blocker offers a two-for-one. Also, a cardiologist's familiarity with beta-blockers is high due to their frequency of prescription for these other causes.
- Beta-blockers have a slight “rhythm control” effect i.e. they might reduce the risk of further AF events
- It can be given intravenously for fast effect. So if a patient presents to the emergency department, an intravenous beta-blocker can lead to a quicker slowing of the heart rate. Then conversion and onward prescription to the oral form is to be expected due to the evidenced tolerability.
This evidence applies to patients with heart failure, which is not uncommon in patients with AF but cannot be directly translated over to patients without heart failure. So, it takes us back to the commonly expressed stance in this blog that individual decision-making should be nuanced and each patient should be considered based on their individual characteristics rather than based on a standardised protocol. So the next time rate-control medication (or any medication for that matter) is prescribed, it would be very reasonable (and encouraged) to ask what the alternatives are and the rationale behind the selection of that specific drug.
