The relationship between blood pressure and AF
Hypertension, or high blood pressure, is a significant risk factor for atrial fibrillation, with studies showing that it is present in about 70% AF patients. While the relationship between AF and hypertension is complex, it may alter the structure of the heart, leading to the development of AF.
We are taking on two major public health priorities today and trying to answer these two fundamental questions in five minutes:
- Does AF cause high blood pressure or does high blood pressure cause AF?
- Will treating my high blood pressure reduce my risk of AF?
High blood pressure is the leading driver of strokes and unfortunately, AF isn’t far behind. We know the two combined increase your stroke risk so much that you should be taking a blood thinner regardless of your age, sex, or any other risk factors. You’re at risk.
To answer these questions we will lean heavily on the scientific literature to settle the debates once and for all.
1. High blood pressure causes AF. But sudden onset AF can drop your blood pressure too.
We know the two are associated, i.e. if you have one your chances of developing the other goes up. Population-based studies have shown a really interesting J-shaped relationship between blood pressure and AF risk. If you look at this work from Washington State, you’ll see the odds ratio of having AF increases if your average achieved blood pressure was more than 150mmHg systolic (the bigger number on top) or 95mmHg diastolic (the lesser number at the bottom). The authors rightly tried to mitigate the effects of other risk factors like age, sex, and history of heart attacks to try and isolate the influence of the blood pressure. This study helps put some numbers to the association between high blood pressure and AF risk.
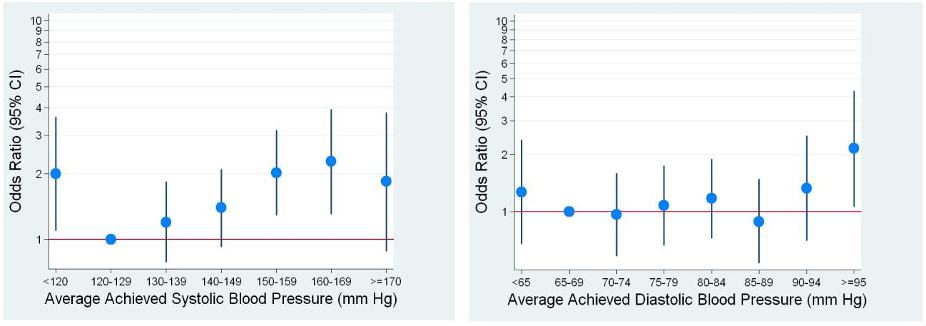
I don’t have a clear explanation for the risk of AF associated with low blood pressure, it may be that patients with low resting blood pressure have a higher risk of other diseases like heart failure or coronary artery disease which increases the AF risk.
But the hard part of this question is attributing causation. A chicken and egg scenario.
But over the years we’ve had some innovative study designs that suggest high blood pressure causes AF rather than the other way around.
If we turn to genetics, we know some genes are associated with high blood pressure (and known not to be associated with AF). So a ‘natural’ randomised controlled trial was done comparing the risk of AF in patients split based on the presence of these BP genes. Elevated blood pressure was associated with an increased risk of atrial fibrillation. Specifically, for every 1 mmHg increase in systolic blood pressure or diastolic blood pressure the relative risk of AF increased by 1.8% and 2.6%, respectively.
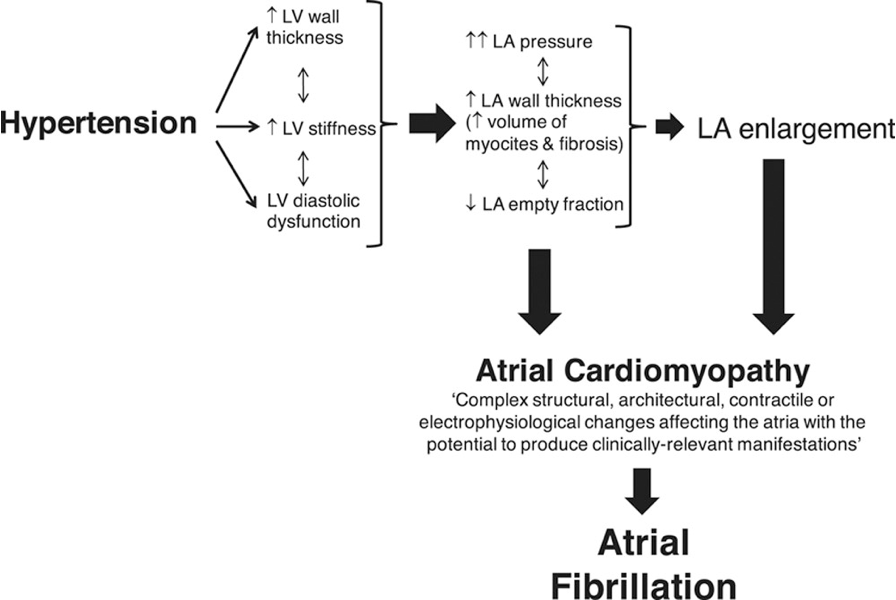
It also makes theoretical sense too. The overly-medicalised diagram below shows that the high pressures cause structural changes in the heart shape, function, and muscle fibres. The changes it causes (like higher pressures and swelling of the top left chamber are known to cause AF and so the chicken and egg cycle starts to look more like a pathway.
In the chronic long-term setting high blood pressure is concerning for AF risk. But in the acute setting, when AF comes on suddenly, doctors will be more concerned when there is low blood pressure, especially if there are symptoms of dizziness or lightheadedness associated with it. This may be because the AF is causing the heart to beat too fast to pump properly and can’t generate pressure to supply the brain. In this case, AF is causing low blood pressure, and medical attention is needed to address the AF.
2. Treating your high blood pressure will reduce your AF risk (and some tablets are better than others!)
So it makes sense to think that reducing that blood pressure would reduce the risk of AF. Indeed the population-based study that showed the J-shaped curve measured the achieved blood pressure in participants i.e. the blood pressure on their prescribed therapy, suggesting that if you can get your blood pressure down your fall into the lower category.
We have studies that show that aggressively controlling blood pressure will reduce your risk of stroke, heart attacks, or heart failure, but the published data on AF is less clear. We have observational-level data (this means studies looking at the relationship with blood pressure and other things incidentally have reported lower AF rates) but I haven't found a randomised controlled trial investigating tighter BP control and AF outcomes.
And we might not get one as well. If you take a step back from the scientific question and think about the impact on patients- should we be studying the value of blood pressure control on AF when we know it leads to so many benefits already?
But there are lots of different types of blood pressure tablets, so a better question might be which one is best for my AF risk. We know some blood pressure tablets have extra effects on reducing AF risk besides bringing down blood pressure. The 'ace-inhibitor' or 'angiotensin receptor blockers (e.g. Ramipril, Enalapril, Candesartan, Valsartan) causes beneficial structural changes in the upper left chamber that originates AF. Studies of patients with heart failure are prescribed these drugs and when they were first rolled out, trialists noticed a lower incidence of new-onset AF in patients on these tablets for their heart failure. This family of tablets has diverse benefits on the risk of future heart attacks if you've had one, the risk of dying if you have heart failure, and the risk of kidney damage- so it's certainly worth discussing the pros and cons with your GP if you need to start taking a blood pressure tablet (this is a really complex decision, so although the ace inhibitors have the benefits I've listed, it also has side effects and so it's always worth getting a personal opinion for your specific situation.
(The Population-based study) Thomas MC, Dublin S, Kaplan RC, Glazer NL, Lumley T, Longstreth WT Jr, Smith NL, Psaty BM, Siscovick DS, Heckbert SR. Blood pressure control and risk of incident atrial fibrillation. Am J Hypertens. 2008 Oct;21(10):1111-6. doi: 10.1038/ajh.2008.248. Epub 2008 Aug 28. PMID: 18756257; PMCID: PMC2577029.
(The Genetics study) Georgiopoulos G, Ntritsos G, Stamatelopoulos K, Tsioufis C, Aimo A, Masi S, Evangelou E. The relationship between blood pressure and risk of atrial fibrillation: a Mendelian randomization study. Eur J Prev Cardiol. 2021 Feb 9:zwab005. doi: 10.1093/eurjpc/zwab005. Epub ahead of print. Erratum in: Eur J Prev Cardiol. 2021 Dec 20;28(14):1617. PMID: 33556963.
