What should we do with AF in the blanking period?

Early AF recurrences can still cause symptoms which should not be ignored
When is the blanking period?
The blanking period is the initial phase after an AF ablation procedure. During this time window, arrhythmias like AF may recur, but they can have different implications on the long-term outcome than recurrences that happen after the blanking period.
Why are these AF recurrences different?
This is because early recurrences may be a result of temporary inflammation of the heart or imbalances in the neurohormones due to the ablation itself. The blanking period has been generally accepted as the first three months after ablation, but recent studies have shown that episodes that occur in that third month are unlikely to resolve on their own, and recent 2024 guidelines have suggested the blanking period be trimmed to two months, with arrhythmias in the third month considered to be unrelated to the procedure.
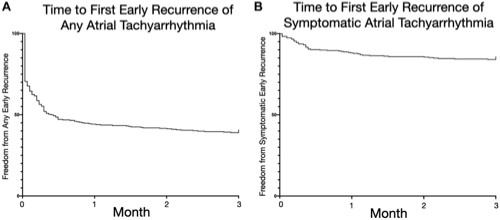
However, early recurrence of atrial tachyarrhythmia (ERAT) is common. If we use implantable, continuous heart rhythm monitors during this period, we see early recurrences in more than 60% of patients.
Early recurrences can still cause problems
Many of these episodes may fizzle out’ and so don’t need any action. However, a small proportion of them will cause troubling symptoms. They can also lead to anxiety and disappointment of the patient who may feel their treatment has failed.
Although catheter ablation is not considered in this early period, this does not mean patients must wait and just tolerate symptoms from arrhythmias that occur in the blanking period. Anti-arrhythmic drugs or electrical cardioversion may be needed to suppress or terminate early recurrence episodes and get patients through.
Anti-arrhythmic drugs for blanking period AF
Anti-arrhythmic drugs can suppress these early recurrences and can reduce symptoms, too. The AMIO-CAT study randomised 212 patients to either amiodarone (a strong anti-arrhythmic drug) or placebo for 2 months after catheter ablation. Participants taking amiodarone were less likely to have arrhythmias during the blanking period (34% of patients in the amiodarone group, 53% of patients in the placebo group), were less likely to need electrical cardioversion and were less likely to require emergency hospitalisation.
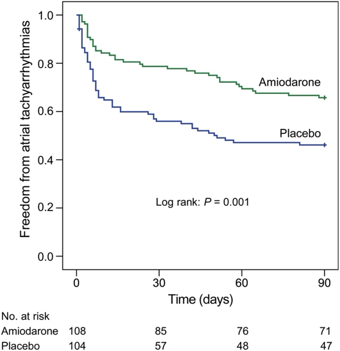
However, the risk of recurrence after the blanking period was not significantly different. Therefore, in practice, anti-arrhythmic drugs are not always used after ablation in the absence of symptoms.
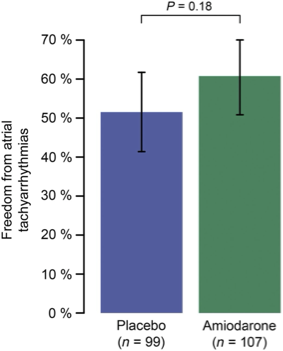
Anti-inflammatory drugs and early recurrence
As early recurrences may be a result of inflammation, specific anti-inflammatory drugs have been tested during this period. Steroids have an anti-inflammatory effect, and so it was hypothesised may treat the underlying cause for early recurrences directly. Again, a reduction in early recurrences was shown, especially in the number of very early recurrences in the first 72 hours, but this did not significantly alter the risk of longer-term outcomes, and so isn’t used widely.
Cardioversion and early recurrence
AF recurrence can also be persistent (i.e. continuous AF) during the blanking period and occur with or without symptoms. We know that being in AF over time leads to changes in the electrical characteristics of the heart that stabilise and maintain it. Therefore, treating it early (within 30 days of onset) with medications or electrical cardioversion is often recommended and supported by guidelines.
Small studies of electrical cardioversion of persistent AF during this blanking period have been encouraging and suggest it may reduce the likelihood of AF after the blanking period. This may be by interrupting those electrical changes, making later AF onset less likely.
Stroke risk in the blanking period
Although treatment for symptoms during this period should be personalised, this does not apply to anticoagulation. Stroke risk is independent from symptoms and patients are at relatively higher risk in the period immediately after an AF ablation. We know the left atrium can be stunned for up to a few months after normal rhythm is reset and this risks blood clot formation and needs continuous anticoagulation throughout to mitigate this risk. After the blanking period, the decision about continuing blood thinners should be made jointly by the patient and their clinical team after discussing the risks and benefits of their individual situation.
Summary
The key message is that AF during the blanking period is common, and you may correctly be told that these episodes do not reflect procedural failure. However, it is important to report these recurrences to your healthcare team, especially if they are causing symptoms. There is no reason to just tolerate and bear it, as non-ablation treatments can still be given and can have a positive effect.
