Atrial Fibrillation and Dementia
Stroke is the sharp end of the ‘complication spear’ when it comes to Atrial Fibrillation. The two are intimately connected with 25% of strokes attributable to AF.
A stroke is a sudden cerebrovascular (=brain blood vessel) blockage but cerebrovascular blockage can also happen gradually. This is the underlying pathology in dementias, with mental slowness, memory problems and general cognitive decline over time. So is the risk of dementia and cognitive decline associated with AF? And can AF-associated dementia be reversed?
AFib is associated with dementia
There is less data on dementia than on stroke because it is harder to diagnose. It can be done using memory tests and questionnaires but it takes time. The studies that have tested this have shown an association between developing AF and increased dementia risk. A combined analysis of eight studies with 77,000 patients, all with normal cognitive function and no dementia at the start of the studies, found that the 15% of patients who developed AFib had a 40% greater risk of dementia than patients without AF after balancing for other risk factors (age, gender, hypertension, diabetes, previous history of stroke). The included trials were all ‘observational’’. So the authors had to try to balance other risk factors between AF and non-AF patient groups. And so despite the extensive efforts to balance all the factors they reported there may have been other features that they could not measure that meant the AF patients were at higher risk of dementia for other reasons (for example let’s say if they were more likely to be smokers).
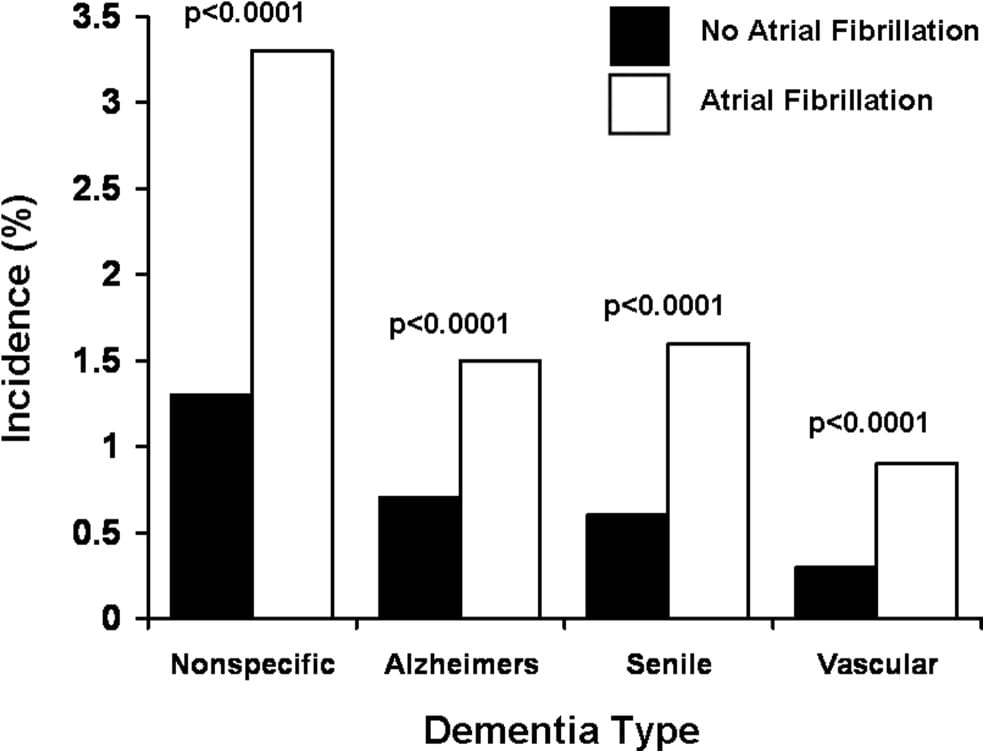
Unfortunately, it is not just vascular dementia risk that's increased. The risk of other types of dementia- Alzheimer’s dementia and senile dementia also appear to be increased in patients with A. The relative risk (the risk of dementia in AF compared to non-AF individuals) appears to be greatest in younger patients.
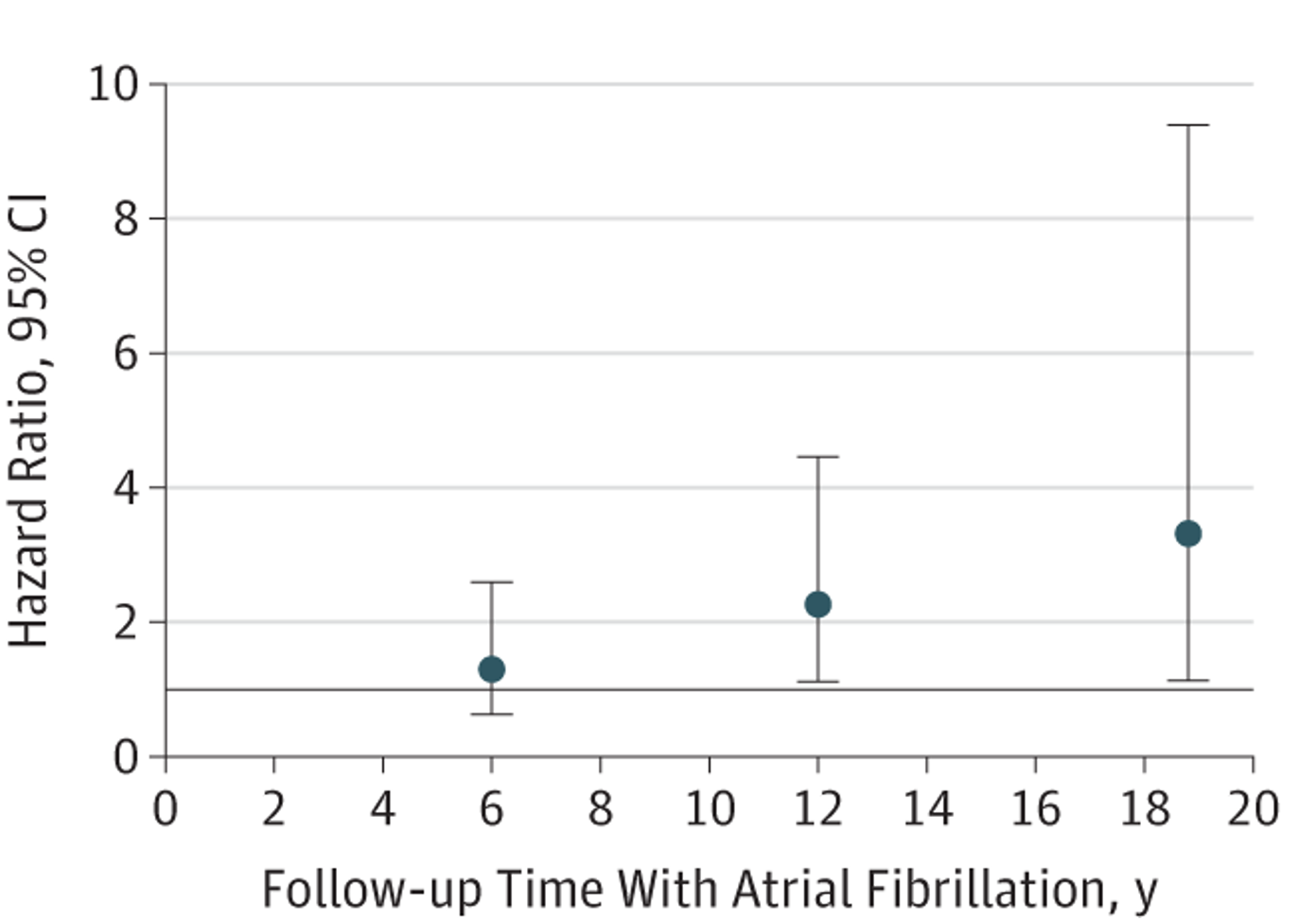
More time in AFib, more dementia
The length of time that an individual is in AFib seems to matter for dementia risk as well. A European study of 6000 participants in the Netherlands found a higher risk of dementia in patients who were in AF (similar to the previous studies). However they also found that in younger participants, individuals with a longer duration of AF had a higher likelihood of AF as well (after balancing for other risk factors).
This could support the argument for early treatment to restore normal rhythm as made in the EAST-AFNET6 trial that showed early rhythm control was associated with improved survival.
Blood thinners reduce the risk of dementia
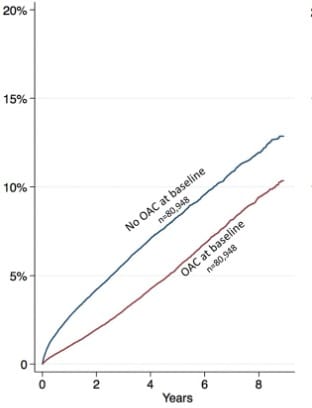
Fortunately, the beneficial effect of blood thinners to reduce stroke in Afib may extend to reducing dementia risk too. A Swedish registry analysis tested this in almost half a million individuals who were diagnosed with AFib between 2006-2014. They compared the rates of dementia between patients who started the blood thinner immediately versus those who started it after a delay.
Patients prescribed a blood thinner within 30 days of diagnosis had a 29% lower risk of dementia than the delayed group. Doing a randomised trial of blood thinner versus no blood thinner in AF patients would be unethical given the proven benefits on stroke risk in patients at risk and so observational analyses like this is as good data as we are going to get.
How might AF cause cerebrovascular disease
The studies so far have shown an association between AF and dementia. But not that AF causes dementia. That is much harder to demonstrate in observational studies because it is hard to say whether the AF itself is the cause or if there is an underlying shared driver of AF risk and dementia risk such as a genetic factor.
There have been relatively small studies that have shown that if you treat the AF with catheter ablation, the AF risk reduces to levels similar to that of non-AF patients which would suggest a causative relationship.
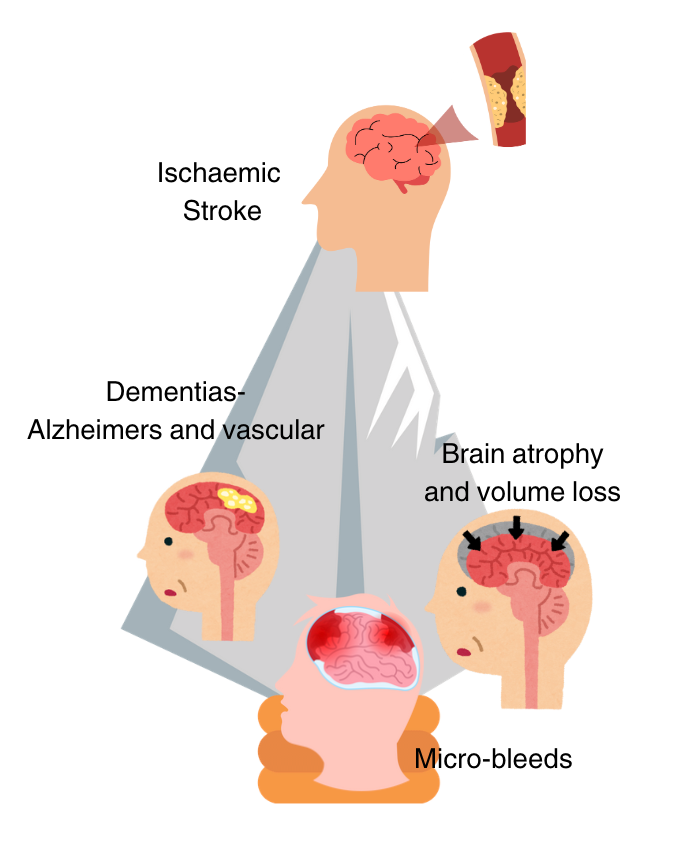
If AF does directly cause dementia, it seems there may be two ways it does this-
One theory is that micro-blood clots form in the fibrillating heart travel up to the brain and cause micro-strokes. As these accumulate over time, you may gradually knock out more brain function leading to cognitive decline and dementia.
A second theory is that the Irregular heartbeats of AF reduce the blood flow to the brain. The brain may get insufficient blood supply during the very fast and very slow beats, leading to a gradual starvation of oxygen and nutrients over time causing dysfunction leading to dementia.
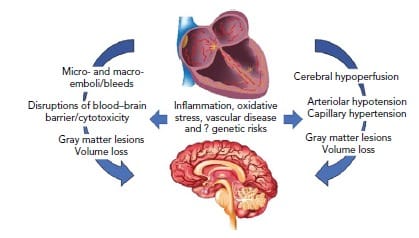
The mechanism is important to understand because it could guide treatment strategies. If it is about micro-blood clots, perhaps the thresholds for starting blood thinners need to be reduced, or perhaps a procedure called ‘left atrial appendage occlusion’ wherein the section of the heart that is most vulnerable to clot development is blocked off is worth investigating as a treatment. If dementia risk is due to the variable heart rate, then medications and procedures that restore normal rhythm should be at the forefront of the treatment strategy and be offered earlier, and perhaps to patients with minimal AF symptoms.
Summary
Stroke is easy to detect using brain scans so diagnosing it is more straightforward than cognitive decline which may slowly progress and can’t be picked up on a brain scan as easily. Therefore it’s likely that stroke may be the tip of the iceberg when it comes to cerebrovascular disease in AFib. The association between AFib and dementia has been shown repeatedly and makes sense. But because it’s hard to measure and more gradual, it doesn’t garner the same attention. However, it can be equally devastating to an affected individual/.
Furthermore, likely, the underlying mechanisms are not limited to just the blood supply to the brain. All organs depend on an efficient blood supply from the heart. Disruption through micro-clots or reduced blood supply may also affect the kidneys, gut and heart itself- but this is even harder to measure. We may be underestimating the consequences of AF by just measuring stroke rates or even cerebrovascular disease rates.
Both AF risk and cerebrovascular/cognitive disease risk share risk factors such as age, diabetes, and high blood pressure. This strengthens the case for risk factor control- if you have high blood pressure, control it, if you are obese, reduce your weight.
In addition, the risk of dementia decreases with anticoagulation in patients with AF and taking it regularly likely reduces the risk of all cerebrovascular diseases, not just stroke.
References
Santangeli P, Di Biase L, Bai R, Mohanty S, Pump A, Cereceda Brantes M, Horton R, Burkhardt JD, Lakkireddy D, Reddy YM, Casella M, Dello Russo A, Tondo C, Natale A. Atrial fibrillation and the risk of incident dementia: a meta-analysis. Heart Rhythm. 2012 Nov;9(11):1761-8. doi: 10.1016/j.hrthm.2012.07.026. Epub 2012 Aug 2. PMID: 22863685.
de Bruijn RF, Heeringa J, Wolters FJ, Franco OH, Stricker BH, Hofman A, Koudstaal PJ, Ikram MA. Association Between Atrial Fibrillation and Dementia in the General Population. JAMA Neurol. 2015 Nov;72(11):1288-94. doi: 10.1001/jamaneurol.2015.2161. PMID: 26389654.
