What should we do with asymptomatic Atrial Fibrillation?
This weekend was the European Society of Cardiology Congress - the largest conference of Cardiologists in the World.

We presented our work characterising differences between asymptomatic versus symptomatic atrial fibrillation- something we have analysed to try and understand what gives some patients terrible symptoms during atrial fibrillation, but others nothing at all.

But first! To frame this question, I want to discuss one of the larger, headline trials presented at the Congress that demonstrates the importance of this topic.
What is the stroke risk of incidentally-detected AF?
1.2-1.4 million cardiac devices (pacemakers, defibrillators, insertable cardiac monitors) are implanted per year. These devices continuously record the heart rhythm. Over their lifetime, about one in five of these patients have fast, irregular heart rhythms detected on their device intermittently. These rhythms would probably look like atrial fibrillation if you did an ECG at the time.
But you need to have an ECG to make the diagnosis of AF. So, strictly speaking, these episodes that are captured on a device and have all the characteristics of AF can't be called AF- they are 'atrial high rate episodes' or AHREs. This may seem pedantic, but we don't yet know if AHREs have the same risks as AF...cue the NOAH-AFNET6 study.
The NOAH-AFNET 6 trial
Blood thinners reduce the risk of stroke in patients with atrial fibrillation.
This benefit is not seen in patients without AF and instead, these patients have an increased risk of bleeding on blood thinners instead.
So where do AHREs sit on this spectrum? Would patients with these episodes benefit from being anticoagulated, just like patients with AF do?
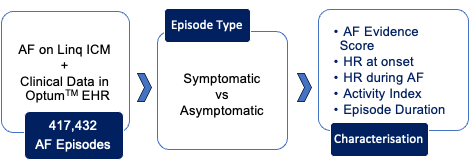
'NOAH-AFNET6' was a 2500-patient randomised controlled trial comparing the use of Edoxaban, a blood thinner versus a placebo (a dummy tablet with no chemical effect) in patients with AHREs.
They enrolled patients from 206 hospitals in 18 countries- a huge undertaking over 6 years. If AHREs had the same stroke risk as AF and benefited from blood thinners in the same way, they expected the stroke rates in the Edoxaban group to be lower than in the placebo group. But this did not happen.
The ground-breaking results showed a similar rate of stroke/blood clot/cardiovascular death rates in both groups of the study. Interestingly the stroke risk was much lower than expected- it was 1% per year, much lower than expected in patients with a moderate risk profile (a CHADSVASc score of 4).
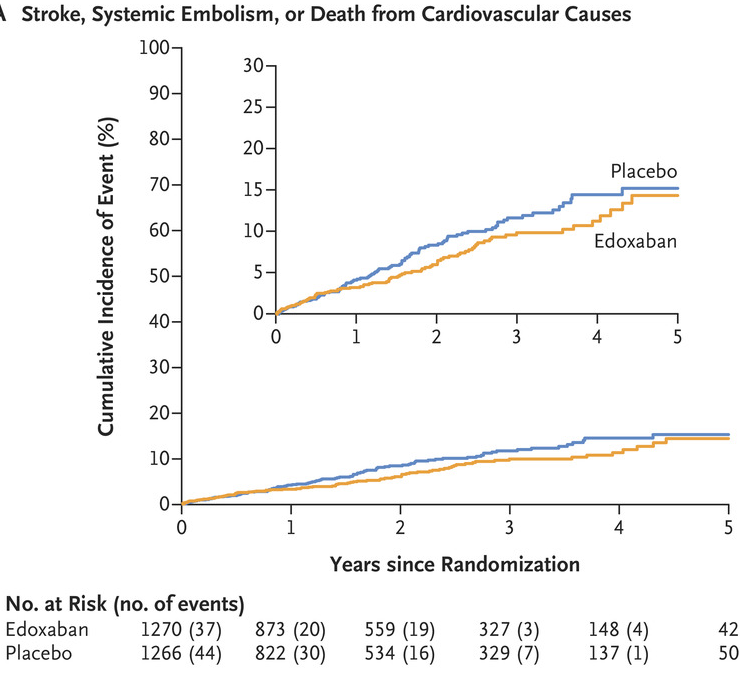
However, the bleeding risk was 30% higher in patients taking the blood thinner and the study supports not anticoagulating patients with AHREs only, unless 'proper' AF is captured on an ECG.
But why is there this difference in stroke risk? What is the difference between AHREs and AF? Understanding these differences has been a research interest of ours at Barts and the NOAH-AFNET6 study set the stage for our work nicely.
What are the differences between symptomatic and asymptomatic AF?
So going back to our original question, are there differences in the pattern of the AF rhythm that lead to some people developing symptoms and other people not? It is an unknown and so the first step for us was to characterise what 'asymptomatic AF' looked like.
99% of patients in NOAH-AFNET6 had pacemaker or defibrillator devices, suggesting underlying cardiac diseases that required them to have these implanted.
1% of their patients had insertable cardiac monitors (ICMs, also referred to as implantable loop recorders or ILRs) which are much smaller devices that are more commonly used for rhythm surveillance only in patients without known cardiac diseases.
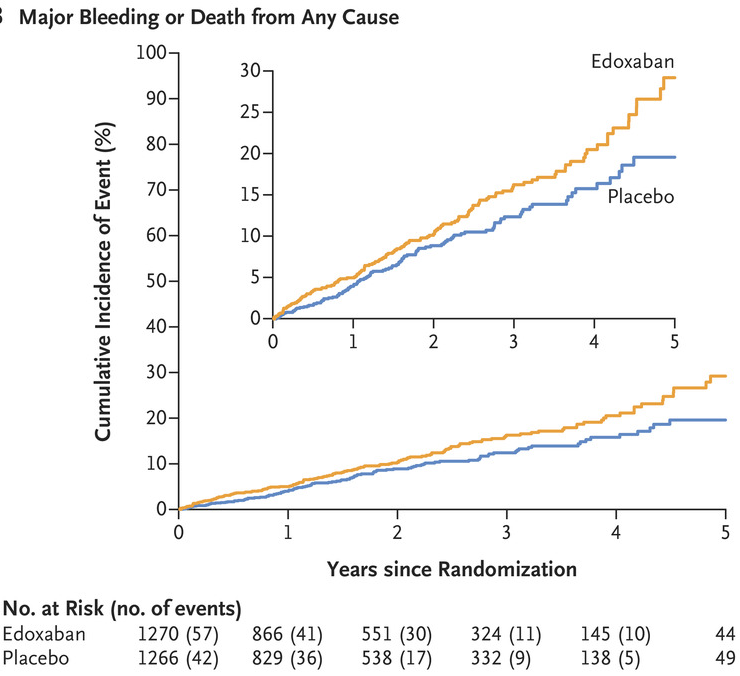
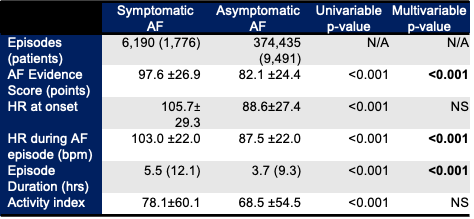
We reached out to the data science team at Medtronic Inc, the largest manufacturer of ICMs and were able to analyse their data from 11,267 patients- a total of 417,432 AF episodes.
Patients are able to label their episodes are symptomatic using a handheld activator button and 15% of patients did this. The rest of the episodes were presumed to be asymptomatic.
Comparing the characteristics of these episodes, we found symptomatic episodes were faster, longer and had a higher irregularity score (the AF evidence score is a mathematical method to measure how irregular the AF rhythm is). We may have expected faster and longer episodes to be associated with symptoms but the increased irregularity of symptomatic episodes is novel and something we are investigating further.
If the irregularity of AF may drive symptoms, could that be something that AF ablation corrects and thus why it can improve symptoms?
You may be thinking- but aren't you analysing AHREs instead of AF? 61% of our patients had a known diagnosis of AF. Our patient population was also quite different- we selected only patients with ICMs who had a much lower prevalence of pre-existing cardiac diseases. However, we need to review the stroke/blood clot/cardiovascular death rates in our patient groups and will be the thing we publish for this group soon!
Kirchhof P, Toennis T, Goette A, Camm AJ, Diener HC, Becher N, Bertaglia E, Blomstrom Lundqvist C, Borlich M, Brandes A, Cabanelas N, Calvert M, Chlouverakis G, Dan GA, de Groot JR, Dichtl W, Kravchuk B, Lubiński A, Marijon E, Merkely B, Mont L, Ozga AK, Rajappan K, Sarkozy A, Scherr D, Sznajder R, Velchev V, Wichterle D, Sehner S, Simantirakis E, Lip GYH, Vardas P, Schotten U, Zapf A; NOAH-AFNET 6 Investigators. Anticoagulation with Edoxaban in Patients with Atrial High-Rate Episodes. N Engl J Med. 2023 Aug 25. doi: 10.1056/NEJMoa2303062. Epub ahead of print. PMID: 37622677.
