Who will get an AF ablation in 2024?
The NHS Commisioning policy for AF ablation has been approved. We will go through the pertinent changes.
The evaluation process
NHS England evaluates commissioning decisions for procedures like AF ablation through a multi-stage process. This involves a selected expert committee made up of doctors, patients and other stakeholders assessing the clinical evidence on effectiveness and safety. They also look at economic evaluations and compare costs with other treatments, considering the potential impact on patients and the wider NHS system. The final decision aims to ensure the best patient outcomes while maintaining cost-effectiveness for the NHS.
They then conduct an engagement process, where the proposed policies are presented for feedback. Relevant groups like the Arrhythmia Alliance- the National Charity for Patients with AF and the British Heart Rhythm Society- representing healthcare professionals caring for AF patients are asked for input.
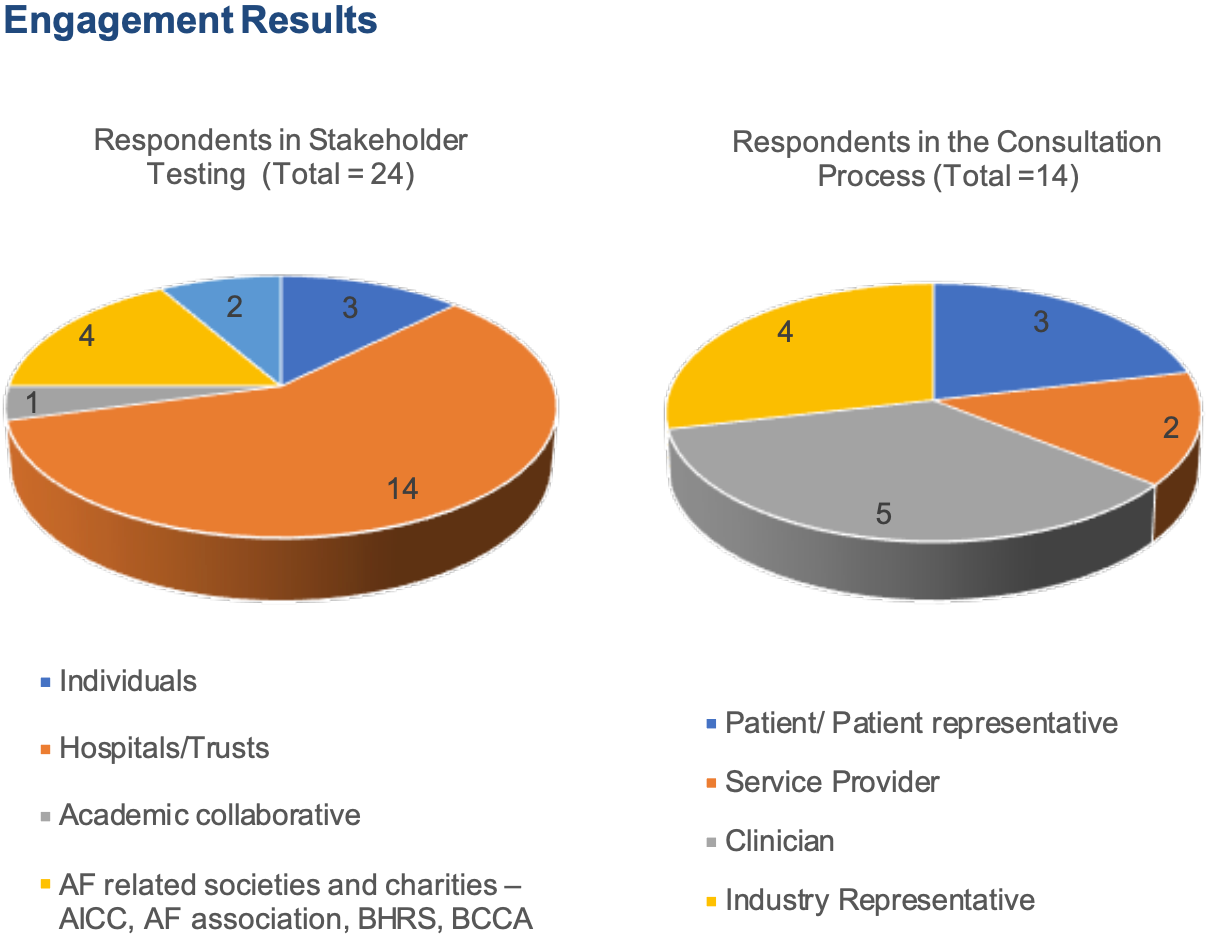
Feedback from 38 stakeholders and 14 patients was sought. Numerous AF studies and articles were presented to try and inform the final output. One primary concern is the need for clarity within the policy's inclusion and exclusion criteria- i.e who should qualify for ablation and who should not.
The final Commissioning policy was published in December 2022 and although it has not come into action, steps are being taken by hospitals to adapt to the new changes. Let’s explore some of these:
You can still get an AF ablation on the NHS if you meet the criteria.
The report conclusion reads:
“NHS England has carefully reviewed the evidence to treat paroxysmal and persistent atrial fibrillation with catheter ablation. We have concluded that there is enough evidence to continue to make the treatment available at this time.”
How much AF matters
You must have had two or more symptomatic AF episodes in the past 6 months lasting a minimum of 60 minutes in total or necessitating admission to hospital.
These symptoms need to be ongoing despite a minimum of three months of antiarrhythmic drug therapy. This can include beta-blockers and calcium channel blockers which aren’t strict anti-arrhythmic drugs and are generally well tolerated.
For patients with persistent AF (continuous AF lasting more than 7 days)- you need to have 2 or more episodes of symptomatic AF in the previous 24 months. (This was originally going to be within 12 months but got extended out to 24 months after the stakeholder feedback).
In the context of patients who have had a cardioversion (the electric shock to reset the heart rhythm), there must be significant improvement in symptoms after the cardioversion. If the patient relapses back into AF, there must be a clear return of their symptoms too.
Persistent AF greater than 2 years in duration is an exclusion criteria- this will affect many patients and means your AF service must be efficient in referral from GP > cardiologist > electrophysiologist > procedure. It is a well-intentioned step as we know long-standing AF is harder to reverse, but it will be interesting to see how a strict cut-off like this is implemented.
Rate control first
Patients in persistent AF who are symptomatic must trial ‘rate control’ first. This should be with one or two agents that slow the heart rate- this can include beta-blockers (bisoprolol, metoprolol), calcium channel blockers (verapamil, diltiazem) or digoxin for atleast 3 months.
Watch your weight
Another clear cut off- Patient with a BMI of greater than 40kg/m2 are not eligible for an AF ablation. If your BMI was between 35-40kg/m2 you would need to undergo intense weight management and demonstrate a weight loss of atleast 10%.
So if you were 5 foot 9 and weighed 125kg you would not be eligible for ablation. If you weighed 108kg, you would have to lose 11kg to be eligible.
Regulating repeat procedures
Repeat procedures should only be considered in patients with ongoing symptomatic episodes of atrial fibrillation or atrial tachycardia recurrence after an AF ablation procedure. However, a third ablation attempt will not be allowed. Under exceptional circumstances a peer review of the case, including an opinion from an expert from an external centre
Special groups
There are additional features that might make you ineligible as well:
- If you have advanced heart failure- classified as NYHA stage 4 heart failure, meaning you experience symptoms even when at rest and are essentially bed-bound.
- Frail patients (classified as more than 'mild' on the Rockwood Clinical Frailty Scale) would have to undergo a comprehensive geriatric assessment to determine whether they would be suitable and how they can be optimised.
- Patients with a life expectancy of less than 5 years
- Patients with Hypertrophic Cardiomyopathy whose AF is persistent.
- Significant heart valve disesase specifically the mitral valve (on the left side of the heart where the AF ablation treatment occurs). This can include severe mitral regurgitation (leak) or stenosis (narrowing) or have a mechanical mitral valve implanted.
Implications
The newly outlined eligibility criteria are designed to select patients with the greatest likelihood of achieving normal rhythm and a noticeable improvement in their symptoms. Whilst patients with a low likelihood of success are steered away and thus not exposed to the small but inevitable possibility of risk too.
NHS England is responsible for optimising the allocation of healthcare resources and ensuring the best possible outcomes for patients. For patients falling into the now ineligible categories, these guidelines might come across as disappointing, perhaps even discriminatory. However, such exclusions often stem from an interpretation of the complexities and nuances associated with treating these specific patient groups. By excluding certain groups where the procedure's risk might outweigh its benefits, it expedites the process of considering alternative, possibly more effective, treatments for them.
For example, patients with persistent AF lasting over two years have a lower chance of achieving normal rhythm in the long term than patients in whom AF is still coming and going. Alternative treatments like 'pace and ablate' may be considered earlier.
Patient focus
One positive is a move towards using patient-centred tools like quality of life surveys. The new guidance also emphasises mandatory patient engagement to demonstate their understanding of what the procedure involves beforehand. All patients must complete this shared decision making tool that explains the rationale of AF ablation and potential risk/benefits.
The AFeQT survey has been licensed by NHS England and must be used to evaluate Quality of Life before and after ablation (something that any patient in the AFFU-AW or AFHF study would be familiar with already)
“Compared with medical therapy, CA appeared to improve AF freedom, reduce hospitalisation and the need for cardioversion. However, there are no benefits in terms of all-cause mortality. In AF patients with heart failure, CA appears to significantly improve LVEF and hospitalisation for worsening HF.”
All the documents including the full Commisioning policy can be found here: https://www.england.nhs.uk/publication/catheter-ablation-for-paroxysmal-and-persistent-atrial-fibrillation-adults/
